Introduction:
Gastroscopy, also known as upper gastrointestinal endoscopy or esophagogastroduodenoscopy (EGD), is a minimally invasive procedure used to examine the inner lining of the upper digestive tract. From diagnosing digestive issues to monitoring treatment effectiveness, gastroscopy plays a crucial role in modern medicine. In this comprehensive guide, we will delve into the intricacies of gastroscopy, its common uses, procedure details, benefits, risks, and advancements in the field.
Understanding Gastroscopy:
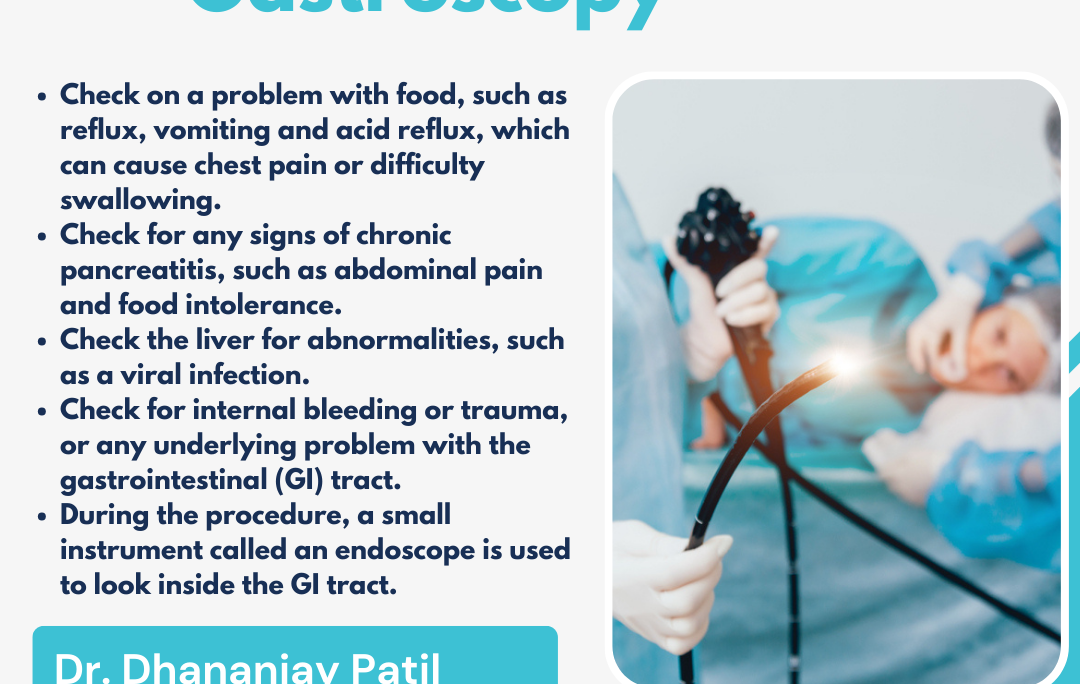
Gastroscopy involves the use of a flexible endoscope, a thin, tube-like instrument with a light and camera attached to its tip. The endoscope is inserted through the mouth and passed down the throat, esophagus, and into the stomach and duodenum. This allows the gastroenterologist to visualize the lining of these organs in real-time, capturing images and videos for examination.
Common Uses of Gastroscopy:
- Diagnosis of Digestive Conditions: Gastroscopy is primarily used to diagnose a wide range of digestive disorders, including gastroesophageal reflux disease (GERD), peptic ulcers, gastritis, Barrett’s esophagus, and esophageal cancer. By directly inspecting the mucous membrane, doctors can identify abnormalities such as inflammation, ulcers, or tumors.
- Evaluation of Symptoms: Patients experiencing symptoms such as persistent heartburn, difficulty swallowing (dysphagia), abdominal pain, nausea, vomiting, or unexplained weight loss may undergo gastroscopy to determine the underlying cause.
- Screening and Surveillance: Individuals at increased risk for certain conditions, such as Barrett’s esophagus or esophageal cancer, may undergo periodic gastroscopy screenings for early detection and monitoring of precancerous changes or abnormalities.
- Treatment and Intervention: Gastroscopy allows for various therapeutic interventions during the same procedure, such as the removal of polyps, dilation of strictures (narrowing), control of bleeding, placement of feeding tubes, or biopsy sampling for further analysis.
Procedure Details:
Before the procedure, patients are usually instructed to fast for several hours to ensure a clear view of the digestive tract. Sedation or anesthesia may be administered to minimize discomfort and promote relaxation during the procedure.
During gastroscopy, the patient lies on their side, and a mouthguard is inserted to protect the teeth and endoscope. The lubricated endoscope is then carefully inserted into the mouth and guided down the throat, allowing the gastroenterologist to navigate through the esophagus, stomach, and duodenum.
Throughout the procedure, the doctor examines the mucosal lining, searching for any abnormalities or lesions. If necessary, tissue samples (biopsies) may be collected using specialized instruments for further analysis under a microscope.
Benefits of Gastroscopy:
- Accurate Diagnosis: Gastroscopy provides direct visualization of the upper digestive tract, enabling doctors to accurately diagnose various conditions and plan appropriate treatment strategies.
- Minimally Invasive: Compared to traditional surgical procedures, gastroscopy is minimally invasive, resulting in shorter recovery times, reduced risk of complications, and minimal scarring.
- Same-day Procedure: Gastroscopy is typically performed as an outpatient procedure, allowing patients to return home on the same day with minimal disruption to their daily activities.
- Versatility: Gastroscopy allows for both diagnostic and therapeutic interventions, making it a versatile tool for managing a wide range of digestive disorders.
Risks and Considerations:
While gastroscopy is generally safe, it may carry certain risks and considerations, including:
- Sedation Risks: Sedatives or anesthesia used during the procedure may cause respiratory depression, allergic reactions, or adverse drug interactions, especially in patients with underlying health conditions.
- Perforation: In rare cases, the endoscope may cause a perforation or tear in the digestive tract lining, leading to infection or bleeding that requires immediate medical attention.
- Bleeding: Biopsy sampling or therapeutic interventions such as polyp removal may result in minor bleeding, which can usually be managed during the procedure.
- Discomfort: Some patients may experience mild discomfort, bloating, or sore throat following gastroscopy, but these symptoms typically resolve within a few hours.
Advancements in Gastroscopy:
Recent advancements in technology have further improved the safety, accuracy, and efficiency of gastroscopy procedures. These include:
- High-definition Imaging: Advanced endoscopes equipped with high-definition cameras provide clearer images of the digestive tract, enhancing visualization and diagnostic accuracy.
- Narrow-band Imaging (NBI): NBI utilizes specific wavelengths of light to enhance the contrast between healthy and abnormal tissue, aiding in the detection of subtle lesions or early-stage cancers.
- Endoscopic Ultrasound (EUS): Combining endoscopy with ultrasound imaging allows for deeper tissue penetration and more accurate staging of gastrointestinal cancers, facilitating targeted treatment planning.
- Capsule Endoscopy: In cases where traditional endoscopy is not feasible, capsule endoscopy involves swallowing a small, pill-sized camera that captures images as it travels through the digestive tract, providing valuable diagnostic information.
Conclusion:
Gastroscopy remains a cornerstone in the diagnosis and management of various digestive disorders, offering a safe, minimally invasive approach to evaluating the upper gastrointestinal tract. With ongoing advancements in technology and techniques, gastroenterologists can continue to provide patients with accurate diagnoses, effective treatments, and improved outcomes. By understanding the uses, benefits, risks, and advancements in gastroscopy, patients and healthcare providers can work together to optimize digestive health and well-being.
#pune #pcmc #chinchwad #hospital #generalsurgeon #gastroscopy #gastroscopytest #endoscopy #endoscopyprocedure #surgery