Back pain is one of the leading reasons people visit a doctor, and a herniated disc is a frequent culprit. Also known as a slipped disc, ruptured disc, or disc prolapse, this condition can cause discomfort ranging from mild aches to severe, disabling pain. The good news? With the right diagnosis and treatment, most people recover fully and return to their normal activities.
1. What is a Herniated Disc?
Your spine is made up of 24 vertebrae (bones) stacked vertically, separated by soft intervertebral discs. These discs act as cushions, absorbing shock and allowing your back to bend and twist.
Each disc has:
- Nucleus pulposus – a soft, gel-like center.
- Annulus fibrosus – a tough, fibrous outer ring.
A herniated disc occurs when the annulus develops a tear or weakness, allowing part of the nucleus to bulge or leak out. If this protrusion presses on nearby spinal nerves, it can cause pain, numbness, or weakness.
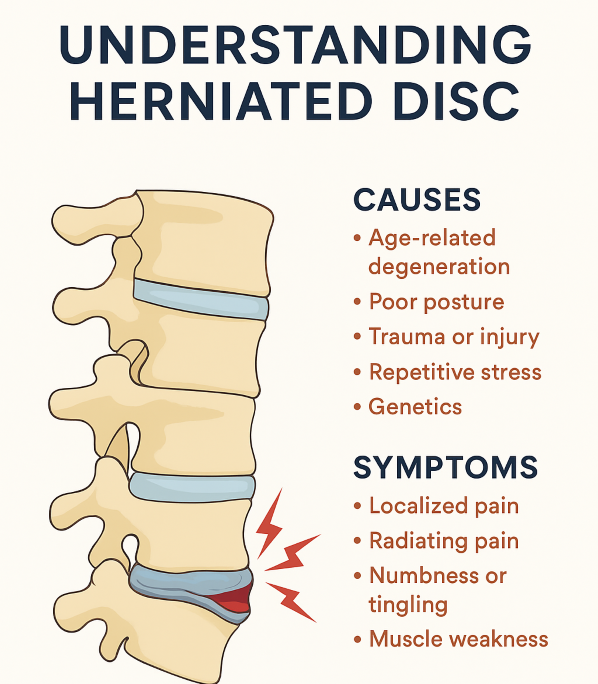
2. Causes of Herniated Disc
Herniated discs usually develop over time due to wear and tear (degenerative disc disease), but they can also occur suddenly. Common causes include:
- Age-related degeneration – Discs lose water content with age, becoming less flexible and more prone to rupture.
- Repetitive strain – Heavy lifting, bending, or twisting motions increase the risk.
- Injury or trauma – Sudden impact from falls, accidents, or sports injuries can cause disc damage.
- Poor posture – Prolonged sitting or incorrect body mechanics put stress on spinal discs.
- Obesity – Excess weight increases the load on the spine.
- Genetics – Some people are more prone to disc problems due to inherited factors.
3. Common Symptoms
Symptoms depend on the location of the herniated disc and whether it presses on a nerve.
Lumbar (Lower Back) Herniation
- Pain radiating from the lower back to the leg (sciatica)
- Tingling or numbness in the leg or foot
- Muscle weakness in the lower extremities
- Pain worsens with sitting, bending, or lifting
Cervical (Neck) Herniation
- Neck pain radiating to the shoulder, arm, or hand
- Tingling or numbness in the arm or fingers
- Weakness in arm muscles
- Stiffness and reduced neck mobility
Emergency Warning Signs:
If you experience loss of bladder/bowel control, severe weakness, or sudden paralysis, seek urgent medical care — these may indicate cauda equina syndrome, a medical emergency.
4. How is a Herniated Disc Diagnosed?
A spine specialist begins with a thorough medical history and physical examination, checking reflexes, muscle strength, and sensation.
Tests may include:
- MRI scan – Best imaging for discs and nerves.
- CT scan – Alternative when MRI isn’t possible.
- X-rays – To rule out fractures or bone issues.
- Nerve conduction tests (EMG/NCV) – Evaluate nerve function.
5. Treatment Options
Most herniated discs improve without surgery. Treatment aims to relieve pain, improve mobility, and prevent recurrence.
A) Non-Surgical Treatment
- Rest & activity modification – Avoid heavy lifting and activities that worsen symptoms.
- Medications – Painkillers, anti-inflammatories, muscle relaxants, or nerve pain medicines.
- Physiotherapy – Exercises to strengthen the back, improve flexibility, and relieve nerve pressure.
- Heat & cold therapy – Helps reduce muscle spasm and inflammation.
- Epidural steroid injections – Reduce inflammation around the nerve roots.
B) Surgical Treatment
Surgery is recommended if:
- Symptoms persist beyond 6–12 weeks of conservative treatment.
- There’s significant nerve compression causing weakness.
- There’s bladder or bowel dysfunction.
Common surgical procedures:
- Microdiscectomy – Removing the herniated part of the disc via a small incision.
- Endoscopic discectomy – Minimally invasive approach using a tiny camera for precision.
- Laminectomy – Removing part of the vertebra to relieve nerve pressure.
Advantages of Endoscopic Surgery:
- Minimal incision (1–2 cm)
- Less muscle damage and blood loss
- Faster recovery — many patients walk within hours
- Shorter hospital stay
6. Recovery & Rehabilitation
Recovery depends on the severity of the herniation and treatment method:
- Post-surgery physiotherapy helps restore muscle strength and posture.
- Ergonomic adjustments at work and home prevent recurrence.
- Gradual return to activity — heavy lifting should be avoided initially.
7. Prevention Tips
While you can’t completely prevent disc problems, you can reduce your risk by:
- Maintaining a healthy weight
- Exercising regularly, focusing on core and back muscles
- Using correct lifting techniques (bend at the knees, not waist)
- Avoiding prolonged sitting or poor posture
- Quitting smoking — nicotine accelerates disc degeneration
8. Living with a Herniated Disc
With the right care, most patients recover without lasting problems. Early diagnosis and treatment are key to avoiding chronic pain or nerve damage.