Introduction Frozen shoulder, also known as adhesive capsulitis, is a debilitating condition that affects the shoulder joint, causing pain, stiffness, and limited range of motion. In this comprehensive guide, we will delve into the causes, symptoms, diagnosis, and various treatment options available for frozen shoulder.
- Anatomy of the Shoulder Joint – To understand frozen shoulder better, it’s crucial to have a basic understanding of the anatomy of the shoulder joint. The shoulder is a complex ball-and-socket joint that allows a wide range of motion, including forward and backward movement, rotation, and elevation. The main bones involved in the shoulder joint are the humerus (upper arm bone), scapula (shoulder blade), and clavicle (collarbone). Surrounding the joint are several muscles, ligaments, and tendons that provide stability and facilitate movement.
- What is Frozen Shoulder? – Frozen shoulder is a condition characterized by inflammation, thickening, and tightening of the capsule surrounding the shoulder joint. This leads to progressive stiffness and pain in the shoulder, making everyday activities like reaching overhead, dressing, or combing hair difficult and painful. The exact cause of frozen shoulder is not fully understood, but several factors can contribute to its development.
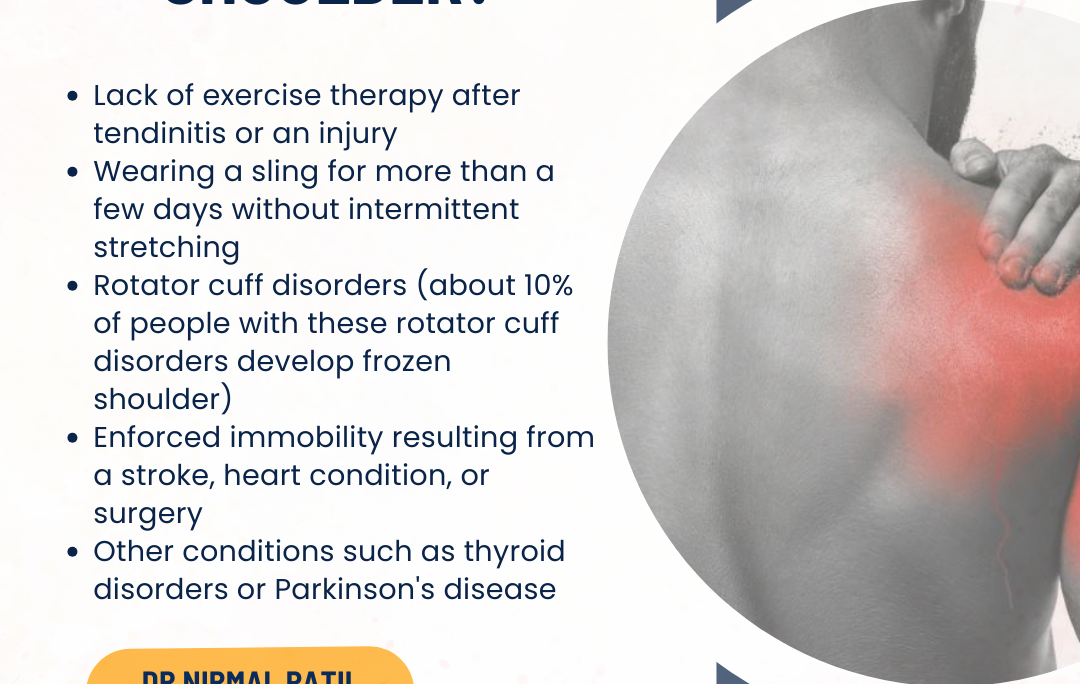
- Causes and Risk Factors – While the exact cause of frozen shoulder remains unclear, certain factors can increase the risk of developing this condition. These risk factors include:
- Age: Frozen shoulder is more common in individuals aged 40 to 60 years.
- Gender: Women are more likely to develop frozen shoulder than men.
- Diabetes: People with diabetes have a higher risk of developing frozen shoulder, possibly due to glucose metabolism affecting the shoulder joint’s tissues.
- Shoulder Trauma or Surgery: Previous shoulder injuries, surgeries, or immobilization can lead to adhesive capsulitis.
- Other Medical Conditions: Certain medical conditions such as thyroid disorders, cardiovascular disease, and autoimmune conditions may increase the risk of frozen shoulder.
- Symptoms of Frozen Shoulder – The symptoms of frozen shoulder typically develop gradually and progress through three distinct stages:
- Freezing Stage: During this stage, patients experience increasing shoulder pain and stiffness, especially at night or with movement. Range of motion starts to decrease.
- Frozen Stage: In this stage, shoulder stiffness becomes more pronounced, making it challenging to perform daily activities. Pain may persist, especially with sudden movements or attempts to reach overhead or behind the back.
- Thawing Stage: In the final stage, shoulder movement gradually improves, and pain subsides. However, this stage can take several months to years to reach full recovery.
- Diagnosis of Frozen Shoulder – Diagnosing frozen shoulder involves a comprehensive evaluation by a healthcare professional, typically a primary care physician or orthopedic specialist. The diagnosis is based on a combination of medical history, physical examination, and imaging studies such as X-rays or MRI scans. Key aspects of the diagnosis include assessing range of motion, identifying specific shoulder movements that cause pain or stiffness, and ruling out other possible causes of shoulder pain and dysfunction.
- Treatment Options for Frozen Shoulder – The management of frozen shoulder aims to relieve pain, improve shoulder mobility, and restore function. Treatment options may vary depending on the severity of symptoms and stage of the condition. Common treatment modalities include:
- Physical Therapy: Gentle stretching exercises, range of motion exercises, and manual therapy techniques performed by a physical therapist can help improve shoulder mobility and reduce stiffness.
- Pain Management: Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to alleviate shoulder pain and inflammation.
- Corticosteroid Injections: Injections of corticosteroids directly into the shoulder joint can help reduce inflammation and provide temporary pain relief.
- Hydrodilatation: This procedure involves injecting a sterile fluid into the shoulder joint to stretch the capsule and improve range of motion.
- Manipulation Under Anesthesia (MUA): In some cases, a healthcare provider may perform a controlled manipulation of the shoulder joint while the patient is under anesthesia to break up adhesions and improve mobility.
- Surgery: Surgical intervention for frozen shoulder is typically considered when conservative treatments have not provided sufficient relief. Procedures such as arthroscopic capsular release or manipulation under anesthesia with capsular release may be performed to release tight tissues and improve shoulder function.
- Self-Care and Home Remedies – In addition to professional medical treatment, individuals with frozen shoulder can benefit from self-care strategies and home remedies to manage symptoms and promote healing. These include:
- Heat and Cold Therapy: Applying heat packs or cold packs to the shoulder can help alleviate pain and reduce inflammation.
- Rest and Avoidance of Overhead Activities: Resting the shoulder and avoiding activities that worsen pain or stiffness can prevent further irritation of the joint.
- Gentle Stretching Exercises: Performing gentle shoulder stretches as recommended by a healthcare provider or physical therapist can help maintain and improve range of motion.
- Proper Posture and Ergonomics: Maintaining good posture and using ergonomic techniques when performing daily tasks can reduce strain on the shoulder joint.
- Healthy Lifestyle Choices: Managing underlying medical conditions such as diabetes, maintaining a healthy weight, and engaging in regular physical activity can support overall shoulder health.
- Prognosis and Recovery – The prognosis for frozen shoulder varies from person to person and depends on factors such as the severity of the condition, adherence to treatment, and individual response to therapy. In many cases, frozen shoulder improves over time with appropriate treatment and rehabilitation. However, full recovery can take several months to years, particularly in severe or chronic cases. It’s essential for patients to follow their healthcare provider’s recommendations, attend physical therapy sessions as prescribed, and practice self-care techniques to optimize recovery and shoulder function.
- Prevention Strategies – While it may not be possible to prevent frozen shoulder entirely, certain strategies can help reduce the risk or severity of the condition:
- Maintain a Healthy Lifestyle: Regular exercise, proper nutrition, and weight management can promote overall joint health and reduce the risk of shoulder problems.
- Avoid Prolonged Immobilization: If recovering from shoulder surgery or injury, follow your healthcare provider’s instructions regarding early mobilization and rehabilitation exercises to prevent stiffness and adhesions.
- Manage Underlying Medical Conditions: If you have diabetes or other medical conditions associated with frozen shoulder risk, work closely with your healthcare team to manage these conditions effectively.
Conclusion – Frozen shoulder, or adhesive capsulitis, is a challenging condition that can significantly impact shoulder function and quality of life. Understanding the causes, symptoms, diagnosis, and treatment options for frozen shoulder is essential for individuals affected by this condition and their healthcare providers. With appropriate medical care, physical therapy, and self-care strategies, many individuals can achieve improved shoulder mobility and pain relief, leading to a better quality of life. If you are experiencing shoulder pain, stiffness, or limited range of motion, consult with a healthcare professional for evaluation and personalized treatment recommendations.
#hospital #pune #pcmc #chinchwad #medical #medicalservices #frozenshoulder #frozenshouldertreatment #adhesivecapsulitis #frozenshouldertherapies #shoulderpain #jointpain #shoulderinjury #shoulder #shoulderpainrelief #shoulderpaindoctor #shoulderjointpain #leftshoulderpain #rightshoulderpain #orthopaedic #shoulderarthritis