Allergic conjunctivitis is a common eye condition that affects millions of people worldwide. It is characterized by inflammation of the conjunctiva, the thin membrane that covers the white part of the eye and lines the inner surface of the eyelids. This condition can cause discomfort, itching, redness, and watery discharge in the eyes. In this comprehensive guide, we will delve into the causes, symptoms, diagnosis, and treatment options for allergic conjunctivitis.
What Causes Allergic Conjunctivitis?
Allergic conjunctivitis is primarily triggered by exposure to allergens. These allergens can vary depending on the individual and the specific type of allergic conjunctivitis. The main types of allergic conjunctivitis include:
- Seasonal Allergic Conjunctivitis (SAC): This type of conjunctivitis occurs seasonally and is often triggered by outdoor allergens such as pollen from trees, grasses, and weeds. Seasonal changes can lead to increased pollen levels in the air, exacerbating symptoms in susceptible individuals.
- Perennial Allergic Conjunctivitis (PAC): Unlike SAC, PAC can occur throughout the year and is usually associated with indoor allergens like dust mites, pet dander, mold, and certain fabrics or cosmetics.
- Vernal Keratoconjunctivitis (VKC): VKC is a more severe form of allergic conjunctivitis that typically affects children and young adults. It is commonly seen in warm climates and is linked to allergens such as pollen, dust, and exposure to certain eye drops or contact lens solutions.
- Atopic Keratoconjunctivitis (AKC): AKC is a chronic and severe form of allergic conjunctivitis that is often associated with atopic dermatitis (eczema) and asthma. It can cause significant discomfort and may lead to corneal complications if not properly managed.
- Giant Papillary Conjunctivitis (GPC): GPC is commonly seen in contact lens wearers and is characterized by the formation of large papillae (bumps) on the inner surface of the eyelids. It is triggered by the chronic irritation caused by contact lenses or eye prostheses.
Symptoms of Allergic Conjunctivitis
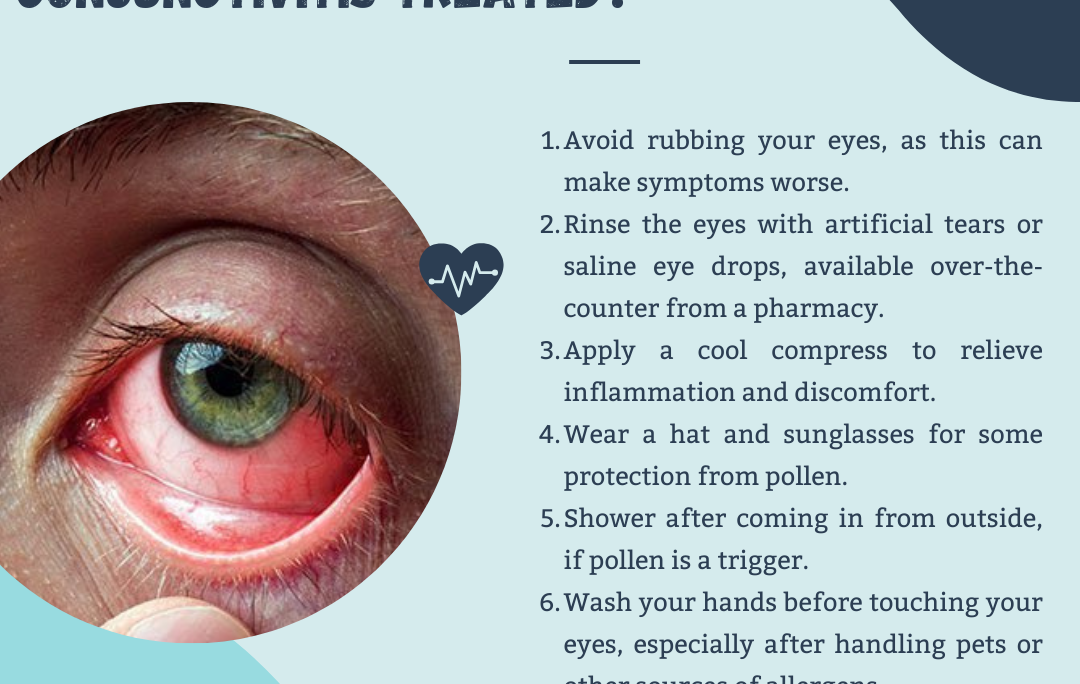
The symptoms of allergic conjunctivitis can vary in severity and may include:
- Itching: One of the hallmark symptoms of allergic conjunctivitis is intense itching in the eyes, which can be very bothersome and disruptive to daily activities.
- Redness: The eyes may appear red or bloodshot due to inflammation of the conjunctiva and dilation of blood vessels.
- Watery Discharge: Allergic conjunctivitis can cause a clear or watery discharge from the eyes, leading to a constant tearing or watering sensation.
- Swelling: The eyelids may become swollen or puffy, especially in cases of severe allergic reactions.
- Grittiness or Foreign Body Sensation: Some individuals with allergic conjunctivitis may experience a sensation of having something gritty or foreign in their eyes.
- Photophobia: Sensitivity to light (photophobia) is another common symptom, where bright light sources can exacerbate eye discomfort.
- Blurry Vision: In severe cases or if the cornea becomes affected, allergic conjunctivitis may cause blurry vision or difficulty focusing.
Diagnosis of Allergic Conjunctivitis
Diagnosing allergic conjunctivitis typically involves a comprehensive eye examination by an ophthalmologist or optometrist. The healthcare provider will review the patient’s medical history, ask about symptoms, and perform a series of tests to assess the eyes’ condition. These tests may include:
- Visual Acuity Test: This test measures how well the patient can see at various distances using an eye chart.
- Slit-Lamp Examination: A slit lamp is a specialized microscope that allows the doctor to examine the structures of the eye, including the conjunctiva, cornea, iris, and lens.
- Allergy Testing: In cases where specific allergens are suspected to be the triggers, allergy testing such as skin prick tests or blood tests (RAST) may be conducted to identify the allergens responsible for the allergic reaction.
- Tear Film Evaluation: The doctor may assess the quantity and quality of tears produced by the eyes, as dry eye syndrome can sometimes mimic allergic conjunctivitis.
Treatment Options for Allergic Conjunctivitis
The management of allergic conjunctivitis aims to alleviate symptoms, reduce inflammation, and prevent recurrences. Treatment options may vary depending on the type and severity of conjunctivitis, as well as the individual’s overall health. Common treatment strategies include:
- Avoidance of Allergens: Whenever possible, avoiding exposure to known allergens can help reduce the frequency and severity of allergic reactions. This may involve staying indoors during high pollen seasons, using allergen-proof covers on pillows and mattresses, and minimizing contact with pets or other allergenic substances.
- Topical Antihistamines: Over-the-counter or prescription eye drops containing antihistamines can help relieve itching and redness by blocking histamine receptors in the eyes. Examples include ketotifen, olopatadine, and azelastine eye drops.
- Topical Mast Cell Stabilizers: Mast cell stabilizer eye drops work by preventing the release of histamine and other inflammatory mediators from mast cells in the conjunctiva. These drops are often used as maintenance therapy to prevent allergic reactions. Common mast cell stabilizers include cromolyn sodium and nedocromil.
- Topical Corticosteroids: In cases of severe allergic conjunctivitis or when other treatments are ineffective, short-term use of topical corticosteroid eye drops may be prescribed to reduce inflammation and control symptoms. However, prolonged use of corticosteroids carries risks of side effects such as increased intraocular pressure and cataract formation, so they are typically used under close supervision by an eye care professional.
- Cold Compresses: Applying cold compresses or cool, damp cloths to the eyes can provide temporary relief from itching, swelling, and discomfort. Cold therapy helps constrict blood vessels and reduce inflammation.
- Contact Lens Management: Individuals with allergic conjunctivitis who wear contact lenses should follow proper hygiene practices and consider switching to daily disposable lenses to reduce the buildup of allergens and bacteria on lens surfaces. In cases of GPC, temporary cessation of contact lens wear may be necessary to allow the eyes to heal.
- Immunotherapy (Allergy Shots): For patients with severe and persistent allergic conjunctivitis that does not respond adequately to other treatments, allergen immunotherapy (allergy shots) may be recommended. Allergy shots involve regular injections of small amounts of allergens to desensitize the immune system over time, reducing allergic reactions.
#hospital #pune #pcmc #chinchwad #medical #medicalservices #dryeyetreatment #dryeyerelief #dryeyedisease#dryeyetherapy #catract #catractsurgery #catracteyesurgery #catracteyeoperation #eyedoctor #glaucoma #conjunctivitis #ophthalmologist #eyediseases #eyepain #pinkeye #myopia #eyeinfection #amblyopia #dryeyesyndrome #eyeproblems #motibindu #motibinduoperation