Pelvic pain is one of the most common concerns among women, yet it is also one of the most ignored. Many women assume that pelvic discomfort is a normal part of the menstrual cycle, stress, or routine physical activity. However, persistent or recurring pelvic pain often has an underlying medical reason—and identifying it early is crucial for proper treatment, long-term health, and overall quality of life.
Pelvic pain refers to discomfort felt in the lower abdomen, below the belly button and between the hips. It can be sudden and sharp or dull and constant. Some women experience pain only during specific activities like menstruation, intercourse, or urination, while others feel it throughout the day. Regardless of its pattern, pelvic pain is a symptom that should never be ignored, because it may be linked to gynaecological, urinary, digestive, or even musculoskeletal conditions.
Understanding What Pelvic Pain Means
Pelvic pain is not a disease by itself—it is a warning sign. The pelvic region contains several organs, including the uterus, ovaries, fallopian tubes, bladder, bowel, and pelvic muscles. Any issue affecting these structures can cause discomfort, which is why identifying the exact cause is essential. Some conditions are harmless and temporary, while others may require medical treatment or surgical intervention.
Ignoring pelvic pain or self-medicating with painkillers may offer temporary relief, but it does not address the root cause. Early diagnosis leads to better outcomes, prevents complications, and helps maintain reproductive health—an important aspect for women in their childbearing years.
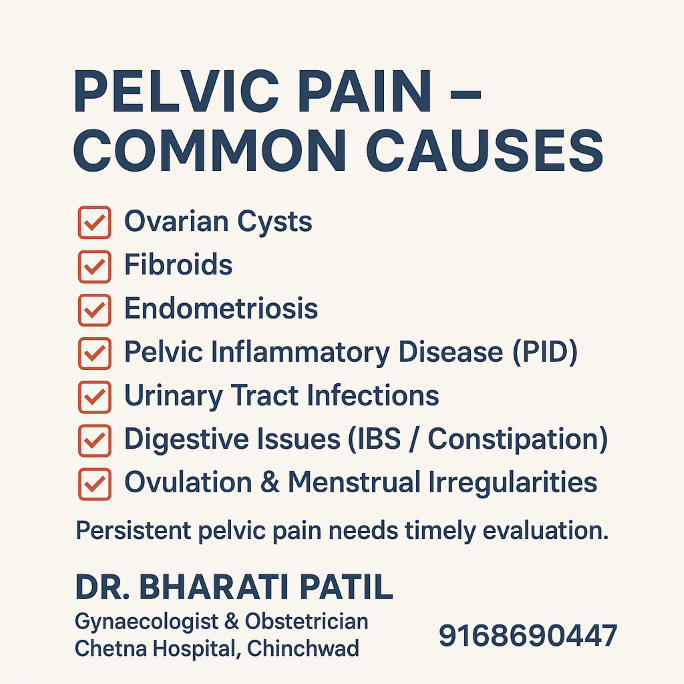
Common Causes of Pelvic Pain
Pelvic pain often arises from gynaecological conditions, but it can also originate from other systems. Below are some of the most common causes:
1. Ovarian Cysts
Ovarian cysts are fluid-filled sacs that develop on the ovaries. Most cysts are harmless, but some may grow larger and cause pain, bloating, backache, or menstrual changes. In rare cases, a cyst may twist (ovarian torsion) or rupture, leading to severe pain and requiring urgent treatment.
2. Uterine Fibroids
Fibroids are non-cancerous growths inside or around the uterus. Depending on their size, number, and location, fibroids may cause pelvic pain, heavy bleeding, painful periods, frequent urination, and difficulty conceiving.
3. Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, such as on the ovaries, fallopian tubes, bladder, or bowel. This condition often leads to severe pelvic pain, especially during periods, and can affect fertility if left untreated.
4. Pelvic Inflammatory Disease (PID)
PID is an infection of the reproductive organs, usually caused by bacteria. Symptoms include pelvic pain, fever, abnormal discharge, irregular periods, and pain during intercourse. If untreated, PID can lead to chronic pain and infertility due to scarring.
5. Urinary Tract Infection (UTI)
UTIs commonly cause burning while urinating, frequent urge to urinate, lower abdominal pain, and pelvic discomfort. While UTIs are easily treatable, ignoring them can lead to kidney involvement and serious complications.
6. Digestive Issues
Sometimes pelvic pain arises from digestive conditions such as Irritable Bowel Syndrome (IBS), constipation, acidity, or inflammation of the intestine. These conditions may cause cramps, bloating, and lower abdominal discomfort.
7. Ovulation or Menstrual-Related Pain
Many women experience brief pain during ovulation (known as mittelschmerz) or cramps during menstruation. While mild pain is normal, severe pain that interferes with daily activities requires medical evaluation to rule out endometriosis, adenomyosis, or hormonal imbalance.
8. Ectopic Pregnancy (Emergency)
This occurs when a fertilized egg implants outside the uterus, usually in the fallopian tube. It can cause sharp pelvic pain, bleeding, dizziness, and requires emergency treatment to prevent life-threatening complications.
When Should You Worry About Pelvic Pain?
Not all pelvic pain is an emergency, but certain signs should prompt immediate medical attention. You should visit a gynaecologist if:
- Pain is severe, sudden, or persistent
- Pain interferes with daily activities
- You experience fever or vomiting along with pelvic pain
- There is abnormal bleeding or discharge
- Pain occurs during intercourse or urination
- You suspect you may be pregnant
- You feel a lump or swelling in the pelvic area
- Pain continues for more than 2–3 days without improvement
Early evaluation helps identify the cause accurately and prevents minor issues from turning into major concerns.
How Is Pelvic Pain Diagnosed?
A gynaecologist begins with a detailed medical history and physical examination. To understand the cause more clearly, the doctor may recommend:
- Ultrasound Scan: To examine uterus, ovaries, and reproductive organs
- Blood Tests: To check for infection, inflammation, or hormonal imbalance
- Urine Tests: To rule out urinary infections
- Pap Smear: To detect cervical abnormalities
- Vaginal Swab: To check for sexually transmitted infections
- Advanced Imaging: Such as CT scan or MRI if required
- Laparoscopy: In certain complex cases for direct examination
These tests help identify the source of pain and guide the correct treatment plan.
Why You Should Not Ignore Pelvic Pain
Ignoring or tolerating pelvic pain can lead to:
- Worsening of infections
- Chronic pelvic pain
- Reduced fertility
- Ovarian cyst complications
- Endometriosis progression
- Difficulty in daily activities and emotional stress
Early diagnosis not only helps with timely treatment but also protects your reproductive health in the long run.
Treatment Options for Pelvic Pain
Treatment depends on the underlying cause and may include:
- Medications: Antibiotics for infections, hormonal therapy, pain relief
- Lifestyle changes: Diet modification, hydration, stress reduction
- Physiotherapy: Pelvic floor rehabilitation for muscle-related pain
- Surgical options: For fibroids, cysts, or endometriosis if needed
- Minimally invasive procedures: Laparoscopy for diagnosis or treatment
Your gynaecologist will recommend the most suitable approach based on your condition.
Conclusion: Listen to Your Body
Pelvic pain is not something to ignore or normalize. It is your body’s way of telling you that something needs attention. Whether mild or severe, recurring or persistent, pelvic pain always has a reason. Consulting a gynaecologist at the right time ensures accurate diagnosis, effective treatment, and long-term relief.
Prioritize your health, listen to your body, and never hesitate to seek help—your well-being matters.