Ovarian inflammation, also known as oophoritis, is a medical condition characterized by the swelling of the ovaries. This inflammation can lead to discomfort, pain, and a range of reproductive health issues. While the condition may not be as commonly discussed as other reproductive health issues, understanding ovarian inflammation is crucial for women’s health. This blog will delve into the causes, symptoms, diagnosis, treatment options, and preventive measures associated with ovarian inflammation.
What Causes Ovarian Inflammation?
Ovarian inflammation can result from various factors, including infections, hormonal imbalances, and underlying medical conditions. Here are some common causes:
- Infections:
- Bacterial Infections: Ovarian inflammation is often caused by bacterial infections, particularly sexually transmitted infections (STIs) like chlamydia and gonorrhea. When these infections are left untreated, they can spread to the ovaries, leading to inflammation.
- Viral Infections: Certain viral infections, such as mumps, can also cause inflammation in the ovaries. Mumps, a contagious viral infection, is less common today due to vaccination but can still lead to complications, including oophoritis.
- Pelvic Inflammatory Disease (PID): PID is an infection of the female reproductive organs, which can occur when STIs spread. This condition can cause the ovaries to become inflamed and is often accompanied by severe pain.
- Endometriosis:
- Endometriosis is a condition where the tissue similar to the lining of the uterus grows outside the uterus, including on the ovaries. This growth can lead to inflammation, pain, and the formation of cysts.
- Hormonal Imbalances:
- Hormonal changes, particularly imbalances in estrogen and progesterone, can affect ovarian function and lead to inflammation. Conditions like polycystic ovary syndrome (PCOS) may also contribute to these hormonal changes.
- Cysts and Tumors:
- Ovarian cysts, which are fluid-filled sacs that can develop on the ovaries, may cause inflammation if they become large, rupture, or become infected. Tumors, both benign and malignant, can also contribute to ovarian inflammation.
- Autoimmune Disorders:
- In some cases, ovarian inflammation may occur as a result of autoimmune disorders where the body’s immune system mistakenly attacks its tissues, including the ovaries.
- Physical Trauma:
- Any physical trauma to the pelvic region, whether from an injury or surgical procedure, can lead to inflammation in the ovaries.
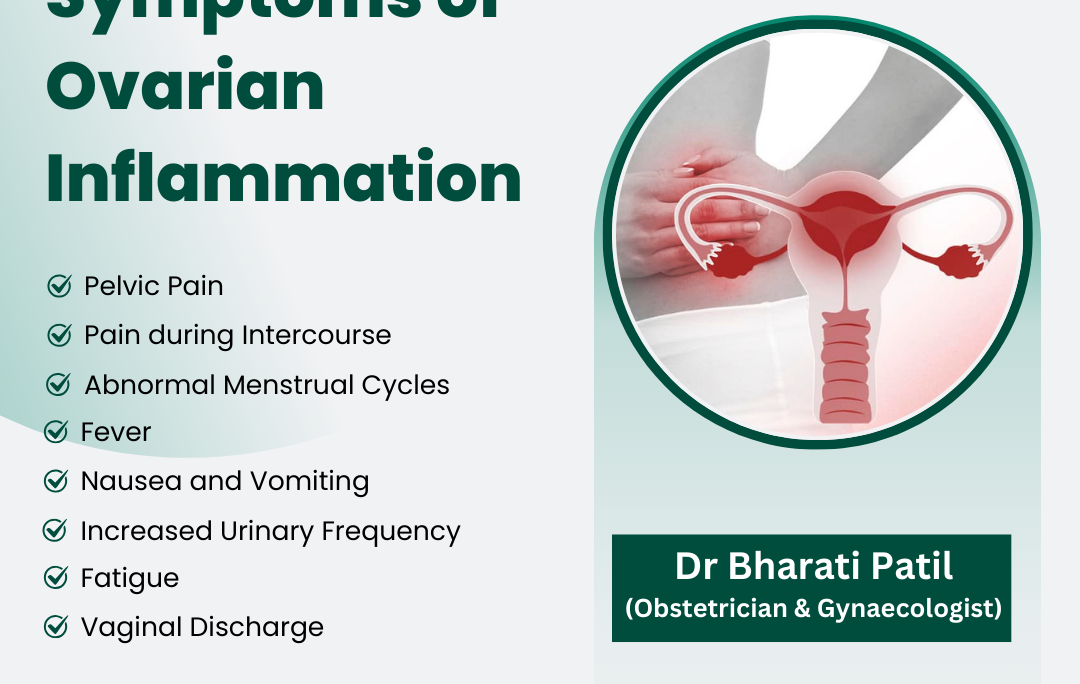
Symptoms of Ovarian Inflammation
The symptoms of ovarian inflammation can vary widely among individuals. While some may experience severe symptoms, others may have mild or no symptoms at all. Common signs include:
- Pelvic Pain:
- Persistent pelvic pain is one of the hallmark symptoms of ovarian inflammation. This pain can range from a dull ache to sharp, intense discomfort, often localized in the lower abdomen. The pain may also radiate to the lower back or thighs.
- Pain During Intercourse:
- Many women with ovarian inflammation experience discomfort or pain during sexual intercourse, which can significantly impact their quality of life.
- Irregular Menstrual Cycles:
- Women may notice changes in their menstrual cycles, including heavier, prolonged, or irregular periods. Some may experience missed periods altogether.
- Abnormal Vaginal Discharge:
- Unusual or foul-smelling vaginal discharge can accompany ovarian inflammation, often indicating an underlying infection.
- Fever and Nausea:
- Fever may develop as the body responds to infection, while nausea can be a result of pain or systemic infection.
- Fatigue:
- Chronic pelvic pain and discomfort can lead to fatigue, affecting daily activities and overall well-being.
- Increased Urinary Frequency:
- Some individuals may experience a frequent urge to urinate, which can occur if the inflammation affects nearby organs.
- Other Symptoms:
- Additional symptoms may include changes in appetite, weight loss, and mood changes.
Diagnosing Ovarian Inflammation
Diagnosing ovarian inflammation involves a thorough medical history, physical examination, and various diagnostic tests. Here’s what to expect during the diagnostic process:
- Medical History:
- The healthcare provider will ask about your medical history, including any previous infections, menstrual cycle irregularities, and any symptoms you may be experiencing.
- Physical Examination:
- A pelvic examination will be performed to check for tenderness, swelling, or abnormalities in the reproductive organs.
- Imaging Tests:
- Imaging tests, such as ultrasound or MRI, may be conducted to visualize the ovaries and surrounding structures. Ultrasound is particularly useful in identifying cysts, tumors, or other abnormalities.
- Blood Tests:
- Blood tests may be ordered to check for signs of infection, inflammation, or hormonal imbalances. Elevated white blood cell counts can indicate infection, while hormonal tests can assess ovarian function.
- Cultures and Other Tests:
- In cases of suspected infection, cultures may be taken to identify specific bacteria or viruses. Additional tests may be needed to rule out other conditions.
Treatment Options for Ovarian Inflammation
The treatment for ovarian inflammation depends on the underlying cause, severity of symptoms, and overall health of the individual. Common treatment options include:
- Antibiotics:
- If the inflammation is caused by a bacterial infection, antibiotics are often prescribed to treat the infection and reduce inflammation.
- Pain Management:
- Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and discomfort. In more severe cases, stronger prescription pain medications may be necessary.
- Hormonal Therapy:
- Hormonal imbalances may be treated with hormonal therapy to help regulate menstrual cycles and alleviate symptoms.
- Surgery:
- In cases where ovarian cysts, tumors, or severe infections are present, surgical intervention may be required. This can involve the removal of cysts, tumors, or even the affected ovary.
- Lifestyle Modifications:
- Maintaining a healthy lifestyle can support overall reproductive health. This includes a balanced diet, regular exercise, and stress management techniques.
- Follow-up Care:
- Regular follow-up appointments are essential to monitor the condition and ensure that treatment is effective.
Preventive Measures
While not all cases of ovarian inflammation can be prevented, certain measures can reduce the risk:
- Practice Safe Sex:
- Using barrier methods, such as condoms, can help prevent sexually transmitted infections that may lead to ovarian inflammation.
- Regular Gynecological Check-ups:
- Routine visits to a healthcare provider can help detect and address any reproductive health issues early.
- Maintain Good Hygiene:
- Practicing good hygiene and cleanliness can reduce the risk of infections.
- Manage Stress:
- Stress can negatively impact overall health, including reproductive health. Engaging in relaxation techniques, such as yoga and meditation, can be beneficial.
- Educate Yourself:
- Understanding your body and recognizing the symptoms of ovarian inflammation can empower you to seek medical attention promptly.
Conclusion
Ovarian inflammation is a significant condition that can impact a woman’s reproductive health and quality of life. Understanding its causes, recognizing the symptoms, and seeking timely medical care are essential for effective management. By prioritizing reproductive health, practicing safe sex, and maintaining a healthy lifestyle, women can reduce their risk of ovarian inflammation and ensure their overall well-being. If you suspect that you may have ovarian inflammation, do not hesitate to consult a healthcare professional for proper evaluation and treatment. Your health matters, and taking proactive steps can lead to a healthier future.
For Consultation Contact us on 9168690447
Website – www.chetnahospital.co.in
Address – Chetna Hospital, Sambhajinagar, MIDC, G Block, Near Rotary Club, Chinchwad 411019
.
.
.
#hospital#pune#pcmc#chinchwad#health#healthcare#gynaecologist#femalegynaecologist#gynaecologistappointment#gynac#gynaecologistdoctor#gynaecologisthospital#goodgynaecologist#gynaecologistspecialist.