Back pain is one of the most common health problems people experience today. While mild discomfort may result from poor posture or muscle fatigue, persistent or radiating pain in the lower back could be a sign of lumbar disc herniation, commonly known as a slipped disc.
The lumbar spine supports most of your body’s weight and allows flexibility in movement. When one of the discs between these lower back bones becomes damaged or slips out of place, it can press against nearby nerves — leading to pain, numbness, or even weakness.
In this article, Dr. Nirmal Patil, Orthopaedic Spine Surgeon, explains what lumbar disc herniation is, its major symptoms, and why early diagnosis is key to preventing long-term complications.
What Is Lumbar Disc Herniation?
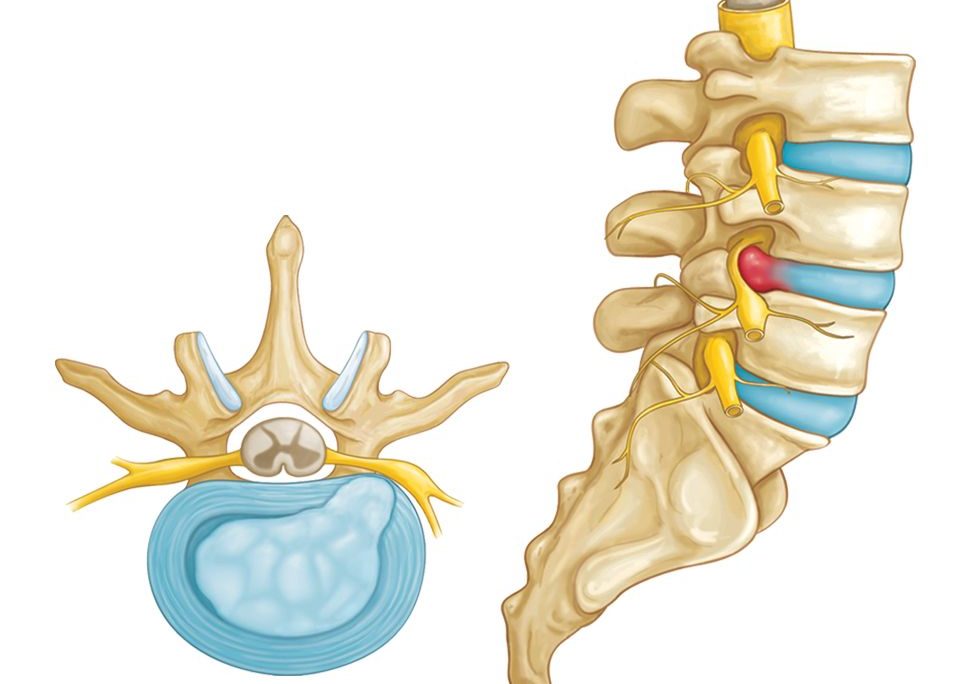
Your spine is made up of a series of bones called vertebrae. Between each vertebra lies a soft, jelly-like cushion called an intervertebral disc, which acts as a shock absorber and provides flexibility to your spine.
When the inner gel-like material of a disc (called the nucleus pulposus) pushes out through the outer layer (annulus fibrosus), it’s known as a disc herniation.
If this occurs in the lower back (the lumbar region), the bulging or ruptured disc may press on nearby spinal nerves — particularly the sciatic nerve, which runs from the lower spine down to the legs.
This nerve compression causes the classic symptoms of lower back pain, leg pain, tingling, and weakness.
Common Causes of Lumbar Disc Herniation
A lumbar disc herniation can develop due to several reasons, including:
- Age-Related Degeneration:
As we age, spinal discs lose water content and elasticity, making them more prone to cracks and ruptures. - Poor Posture:
Sitting hunched over for long hours or maintaining improper posture increases pressure on the lower spine. - Improper Lifting Technique:
Lifting heavy objects by bending your back instead of your knees can strain and damage the discs. - Sudden Movements or Twisting:
Rapid or awkward spinal movements can cause disc injuries. - Obesity:
Extra weight adds constant stress on the lower back. - Lack of Physical Activity:
Weak back and core muscles offer less support to the spine, increasing the risk of disc herniation. - Smoking:
Smoking reduces oxygen flow to spinal tissues, causing early disc degeneration.
Symptoms of Lumbar Disc Herniation
The symptoms of a herniated lumbar disc depend on its severity and the nerves affected. Some people may experience mild pain, while others can have severe nerve-related issues.
Let’s look at the common warning signs:
🩹 1. Persistent Lower Back Pain
The most frequent symptom of lumbar disc herniation is constant lower back pain.
The pain may be dull or sharp and usually worsens during certain activities such as sitting, bending, lifting, or coughing.
Sometimes, the pain may ease when standing or lying flat.
⚡ 2. Leg Pain (Sciatica)
When the herniated disc compresses the sciatic nerve, it causes sciatica — a sharp, burning pain that radiates from the lower back to the buttocks, thighs, calves, and even the feet.
This pain is typically felt on one side and can worsen with movements like sneezing, coughing, or prolonged sitting.
Sciatica is one of the hallmark symptoms of lumbar disc herniation.
🦶 3. Numbness or Tingling Sensation
A compressed nerve cannot send proper signals, leading to numbness, tingling, or a “pins and needles” feeling in the leg or foot.
This sensation often accompanies or follows sciatic pain and usually affects only one side of the body.
💪 4. Muscle Weakness
Continuous pressure on the nerves can weaken the muscles they control.
You might find it hard to lift your foot (known as “foot drop”), stand on your toes, or walk normally.
Muscle weakness is a serious symptom that requires prompt medical attention to prevent permanent damage.
🚨 5. Loss of Reflexes
In some patients, reflexes in the knee or ankle may become sluggish or absent.
A spine specialist often tests this during examination to identify which nerve is compressed.
⚠️ 6. Loss of Bladder or Bowel Control (Emergency Symptom)
In rare but severe cases, the herniated disc can compress the nerves that control bladder and bowel functions, leading to Cauda Equina Syndrome.
Symptoms include loss of bladder/bowel control, numbness in the inner thighs or buttocks, and severe leg weakness.
This is a medical emergency that requires immediate surgical intervention.
When to See a Spine Specialist
You should consult a spine surgeon if you experience any of the following:
- Back pain lasting longer than a few days
- Pain radiating to the legs or feet
- Tingling or numbness in the legs
- Weakness while walking or standing
- Pain that worsens while sitting or bending
- Any loss of bladder or bowel control
Early evaluation by an orthopaedic spine specialist can prevent further nerve damage and improve recovery outcomes.
Diagnosis of Lumbar Disc Herniation
A proper diagnosis involves a combination of medical history, physical examination, and imaging studies.
- Medical History:
The doctor will ask about symptoms, duration, and any activities that worsen the pain. - Physical Examination:
Reflexes, muscle strength, flexibility, and nerve sensitivity are checked to locate the affected area. - Imaging Tests:
- MRI (Magnetic Resonance Imaging): The most accurate test to visualize disc herniation and nerve compression.
- CT Scan or X-ray: Helps assess bone alignment and rule out fractures.
- Nerve Conduction Tests: Measure how well the nerves are functioning.
Treatment Options
Treatment depends on the severity of the herniation and the level of discomfort. Most patients recover with non-surgical methods, but some may require surgical intervention.
💊 1. Conservative (Non-Surgical) Treatment
For mild to moderate cases, conservative management usually provides relief within a few weeks.
It may include:
- Rest and Lifestyle Modification: Avoid heavy lifting or sitting for extended periods.
- Pain Relief Medications: Anti-inflammatory drugs and muscle relaxants reduce discomfort.
- Physiotherapy: Strengthening and stretching exercises improve posture and relieve pressure on the discs.
- Heat or Cold Therapy: Helps ease pain and inflammation.
- Epidural Steroid Injections: Reduce swelling around the affected nerves in severe cases.
Consistent follow-up is essential to monitor progress and prevent recurrence.
🔍 2. Surgical Treatment
If symptoms persist despite conservative care or if there’s significant nerve compression, surgery may be necessary.
Common surgical options include:
- Endoscopic Spine Surgery:
A minimally invasive approach using a small incision and camera-guided instruments to remove the herniated disc portion. Patients usually walk within hours and recover quickly. - Microdiscectomy:
Removal of the damaged part of the disc under a microscope to relieve pressure on the nerve. - Spinal Fusion:
In advanced cases, fusion stabilizes two vertebrae to prevent motion at the damaged level.
Dr. Nirmal Patil, Orthopaedic Spine Surgeon, is highly experienced in endoscopic and minimally invasive spine surgeries, offering patients faster recovery, less pain, and minimal scarring.
Tips to Prevent Lumbar Disc Herniation
You can significantly reduce your risk by following simple lifestyle habits:
- Maintain a healthy body weight to reduce spinal stress.
- Exercise regularly — focus on stretching and strengthening the back and core muscles.
- Practice good posture while standing, sitting, and working.
- Use ergonomic furniture if you sit for long hours.
- Avoid smoking, as it accelerates disc degeneration.
- When lifting heavy objects, bend at the knees and keep your back straight.
Conclusion
Lumbar disc herniation is a common yet treatable condition. Recognizing its early symptoms — such as persistent back pain, radiating leg pain, numbness, or weakness — can help prevent long-term complications.
Ignoring these warning signs or relying solely on painkillers may lead to nerve damage and mobility issues.
If you’re struggling with constant back or leg pain, seek expert consultation from a qualified Orthopaedic Spine Surgeon like Dr. Nirmal Patil. With accurate diagnosis and advanced treatment, you can return to a pain-free and active life.