Introduction
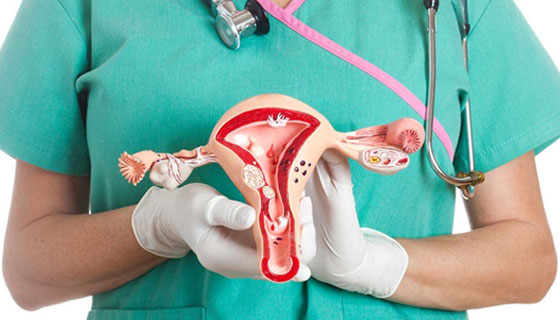
Hysterectomy is a surgical procedure that involves the removal of the uterus, and in some cases, other reproductive organs such as the ovaries and fallopian tubes. It is one of the most common surgical procedures performed on women and is often recommended to treat various medical conditions affecting the uterus. In this blog post, we will delve into the details of hysterectomy, including the different types, reasons for undergoing the procedure, what to expect during recovery, and essential aftercare tips.
Reasons for Hysterectomy
Hysterectomy is recommended by healthcare providers for several medical conditions that affect the uterus and reproductive system. Some of the primary reasons include:
- Uterine Fibroids: Non-cancerous growths in the uterus that can cause heavy menstrual bleeding, pelvic pain, and pressure symptoms.
- Endometriosis: A condition where the tissue lining the uterus (endometrium) grows outside the uterus, leading to pain, infertility, and menstrual irregularities.
- Uterine Prolapse: When the uterus slips from its normal position into the vaginal canal, causing discomfort and urinary incontinence.
- Gynecologic Cancers: In cases of uterine, ovarian, or cervical cancers, hysterectomy may be part of the treatment plan.
- Chronic Pelvic Pain: Persistent pelvic pain that does not respond to other treatments.
Types of Hysterectomy
There are different types of hysterectomy procedures based on the extent of organ removal and surgical approach:
- Total Hysterectomy: Removal of the uterus and cervix.
- Partial Hysterectomy (subtotal or supracervical): Removal of the uterus while leaving the cervix intact.
- Radical Hysterectomy: Removal of the uterus, cervix, part of the vagina, and surrounding tissues (usually performed for gynecologic cancers).
- Surgical Approaches: Hysterectomy can be performed abdominally (open surgery), vaginally, laparoscopically (minimally invasive), or robotically assisted.
Preparing for Hysterectomy
Before undergoing a hysterectomy, patients will undergo a thorough evaluation and preparation process:
- Medical Evaluation: Consultation with a gynecologist or specialist to discuss the reasons for hysterectomy, review medical history, and perform necessary tests (blood tests, imaging studies, etc.).
- Discussion of Options: Patients will be informed about the type of hysterectomy recommended, the surgical approach, potential risks, benefits, and alternatives.
- Preoperative Instructions: These may include fasting before surgery, discontinuing certain medications (such as blood thinners), and preparing for post-operative care and recovery.
- Emotional Preparation: Acknowledging and addressing any emotional concerns or anxieties related to the procedure and its outcomes.
The Hysterectomy Procedure
On the day of the surgery, patients will be admitted to the hospital or surgical center. The steps involved in a hysterectomy procedure depend on the type and approach:
- Anesthesia: Patients are given anesthesia to ensure they are comfortable and pain-free during the surgery.
- Incision: Depending on the surgical approach, incisions are made either abdominally, vaginally, or using minimally invasive techniques (laparoscopy or robotic-assisted).
- Organ Removal: The surgeon carefully removes the uterus and any additional structures as indicated by the type of hysterectomy.
- Closure: After the removal is complete, incisions are closed using sutures or surgical staples.
Recovery Phase
After the surgery, patients are moved to a recovery area where they are closely monitored by medical staff. The recovery period involves several aspects:
- Pain Management: Pain medications are provided to manage post-operative pain and discomfort.
- Hospital Stay: The length of hospital stay varies depending on the type of hysterectomy and individual recovery progress.
- Physical Activity: Initially, patients are advised to rest and limit physical activity. Gradual movement and walking are encouraged as tolerated.
- Follow-up Care: Patients receive instructions for wound care, medication schedules, and follow-up appointments with their healthcare provider.
Follow-up Care and Monitoring
After discharge from the hospital, patients continue their recovery at home and follow specific guidelines:
- Follow-up Appointments: Scheduled appointments with the healthcare provider for post-operative check-ups, monitoring healing progress, and addressing any concerns.
- Activity Graduation: Guidance on resuming normal activities, including work, exercise, and sexual activity, based on individual recovery timelines.
- Monitoring for Complications: Patients are educated about warning signs of complications such as infection, excessive bleeding, or changes in symptoms that require immediate medical attention.
Lifestyle Changes and Long-Term Effects
Hysterectomy can bring about changes in hormonal balance and overall health. Patients are advised on:
- Menopause Management: For women who undergo removal of the ovaries (oophorectomy), hormonal changes leading to menopause may occur. Hormone replacement therapy (HRT) or other medications can help manage menopausal symptoms.
- Bone Health: Addressing bone density and calcium intake to reduce the risk of osteoporosis post-menopause.
- Sexual Health: Open discussions about sexual function, libido changes, and strategies for maintaining intimacy post-hysterectomy.
Risks, Complications, and Safety Measures
While hysterectomy is generally safe, there are potential risks and complications to be aware of:
- Surgical Risks: Infection, bleeding, anesthesia reactions, and organ damage are rare but possible during surgery.
- Long-term Effects: Potential long-term effects such as changes in bowel or bladder function, pelvic organ prolapse, or sexual dysfunction may occur.
- Safety Measures: Surgical techniques, pre-operative assessments, and post-operative care protocols are designed to minimize risks and ensure patient safety.
#hospital #pune #pcmc #chinchwad#health #healthcare #gynaecologist #femalegynaecologist #gynaecologistappointment #gynac #gynaecologistdoctor #gynaecologisthospital #goodgynaecologist #gynaecologistspecialist