Thyroid swelling, commonly known as goitre, is one of the most frequent conditions affecting the thyroid gland. The swelling may be mild and harmless, or it may indicate a serious underlying issue requiring medical intervention. While many thyroid swellings can be managed with observation or medication, certain cases demand timely surgery to avoid complications. Understanding when thyroid swelling becomes a surgical concern is essential for ensuring proper treatment and long-term health.
In this guide, we explore the causes, symptoms, diagnosis, and—most importantly—the situations where thyroid surgery (thyroidectomy) becomes necessary.
🔍 What Is Thyroid Swelling?
The thyroid gland is a small, butterfly-shaped organ located at the front of the neck. It plays a vital role in controlling metabolism, heart rate, digestion, temperature, and overall energy levels by producing hormones (T3 and T4). Thyroid swelling occurs when the gland becomes enlarged due to various reasons, including hormonal imbalance, inflammation, nodules, or cancer.
A thyroid swelling may be:
- Diffuse (entire gland enlarged)
- Nodular (one or multiple lumps)
- Painful or painless
- Small or large enough to cause visible deformity
Most cases are benign, but it is important not to ignore persistent or progressive swelling.
🧠 Common Causes of Thyroid Swelling
Thyroid swelling can develop for several reasons, such as:
1. Iodine Deficiency
Worldwide, iodine deficiency is one of the leading causes of goitre. The thyroid attempts to compensate by enlarging in order to produce adequate hormones.
2. Thyroid Nodules
Nodules are lumps that form within the thyroid gland. They may be:
- Benign (non-cancerous)
- Malignant (cancerous)
- Hot or cold nodules based on activity
Some nodules remain stable, while others grow and cause symptoms.
3. Thyroiditis
Inflammation of the thyroid may be due to autoimmune diseases (e.g., Hashimoto’s thyroiditis), infections, or postpartum hormonal changes. This may cause temporary swelling and pain.
4. Hyperthyroidism
Conditions such as Graves’ disease lead to overactive thyroid function, causing swelling along with symptoms like weight loss, tremors, or palpitations.
5. Hypothyroidism
Even low thyroid function may cause enlargement due to continuous stimulation by the pituitary gland.
6. Thyroid Cancer
Although less common, thyroid cancer typically presents as a nodule or swelling and requires early surgical management.
🔎 Symptoms That Accompany Thyroid Swelling
Some thyroid swellings cause no symptoms, while others may lead to:
- Visible neck bulge
- Difficulty swallowing
- Breathing difficulty
- Hoarseness or voice changes
- Coughing
- Neck tightness
- Pain or discomfort
Symptoms depend on the size, location, and cause of the swelling.
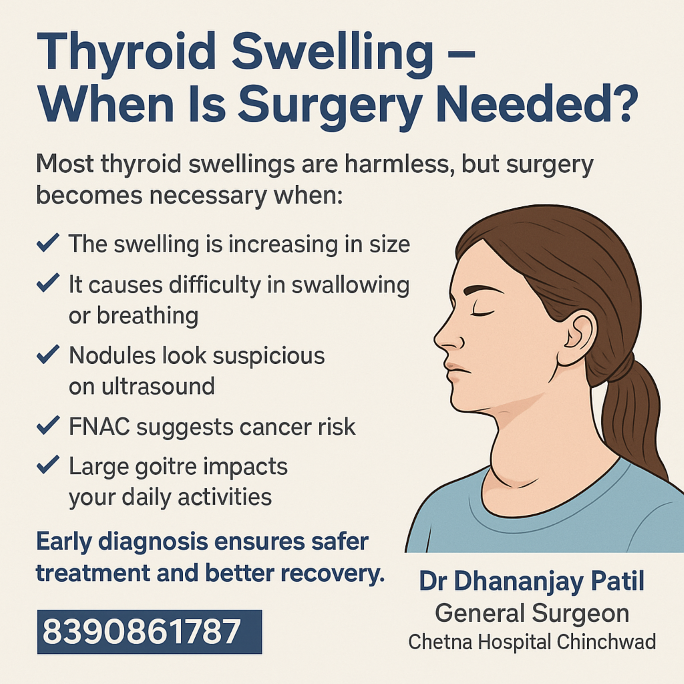
🩺 When Is Surgery Needed?
Not all thyroid swellings require surgery. Many are managed through regular follow-ups, medications, or lifestyle changes. However, surgery becomes necessary in specific situations to prevent complications or treat underlying conditions effectively.
Below are the major indications for thyroidectomy (partial or total removal of the thyroid gland):
1. Increasing Size of the Swelling
A thyroid swelling that continues to grow is a major red flag. Rapidly enlarging swellings may indicate:
- Aggressive nodules
- Cancer
- Internal bleeding into a nodule
- Progressive goitre
Progressive enlargement can compress nearby structures, causing discomfort or breathing issues.
2. Difficulty in Swallowing or Breathing
A large thyroid gland can press against:
- The windpipe (trachea)
- The oesophagus (food pipe)
This may cause:
- Breathing difficulty
- Wheezing
- Trouble swallowing food
- Feeling of choking, especially when lying down
In such cases, surgery is recommended to relieve compression and restore normal function.
3. Suspicious Nodules on Ultrasound
Thyroid ultrasound is an essential diagnostic tool. Nodules that show suspicious features such as:
- Irregular borders
- Microcalcifications
- Taller-than-wide shape
- Internal blood flow
may indicate malignancy. Such nodules often require surgical removal even before biopsy results confirm the diagnosis.
4. FNAC Suggests Cancer or High Suspicion
FNAC (Fine Needle Aspiration Cytology) is a simple and effective test used to evaluate thyroid nodules.
Surgery becomes necessary if:
- Cancer is confirmed
- FNAC reveals “suspicious for malignancy”
- High-risk features are detected
Thyroid cancer has excellent outcomes when treated early with surgery.
5. Large Goitre Affecting Daily Life
Sometimes, even benign swellings cause significant symptoms:
- Visible cosmetic deformity
- Neck tightness
- Persistent discomfort
- Pressure on nerves or vessels
If the goitre affects quality of life or daily activities, surgery provides long-term relief.
6. Hyperthyroidism Not Controlled by Medicine
In cases of Graves’ disease or toxic nodular goitre, surgery is recommended when:
- Medication is ineffective
- Patient experiences severe side effects
- Symptoms worsen despite treatment
- Radioactive iodine therapy is not suitable
Surgery helps restore hormonal balance quickly.
🧪 How Doctors Decide If Surgery Is Needed
A thorough evaluation includes:
1. Blood Tests
To assess thyroid hormone levels (T3, T4, TSH).
2. Ultrasound Neck
To check the structure, size, and nature of nodules.
3. FNAC
To confirm benign or malignant nature.
4. CT Scan
For large goitres extending into the chest (retrosternal goitre).
5. Laryngoscopy
To examine vocal cord function before surgery.
🧑⚕️ Types of Thyroid Surgery
Depending on the diagnosis, the surgeon may perform:
✔️ Hemithyroidectomy
Removal of one lobe of the thyroid.
Used for:
- Single nodules
- Small cancers
- Unilateral goitre
✔️ Total Thyroidectomy
Complete removal of the thyroid gland.
Used for:
- Thyroid cancer
- Bilateral goitre
- Severe hyperthyroidism
- Multiple nodules
After total thyroidectomy, lifelong thyroid hormone supplementation is required.
⏳ Recovery After Thyroid Surgery
Most patients recover well and return home within 1–2 days. Common postoperative expectations include:
- Mild throat discomfort
- Temporary voice change in some cases (rare)
- Small scar at the neck (usually heals well)
- Resuming normal activities in about a week
Regular follow-up ensures proper healing and hormone replacement if necessary.
🧩 When to Consult a Surgeon Immediately
Seek medical attention if you notice:
- Any neck swelling
- Rapid growth of swelling
- Difficulty breathing or swallowing
- Sudden voice changes
- Family history of thyroid cancer
- Persistent cough not related to infection
Early diagnosis dramatically improves outcomes.
📌 Conclusion
Thyroid swelling is common and often harmless, but certain symptoms and diagnostic findings indicate the need for surgery. Whether it is due to a suspicious nodule, a compressive goitre, cancer risk, or uncontrolled thyroid activity, timely surgical intervention ensures safety, prevents complications, and improves long-term health.
Understanding when thyroid surgery is necessary helps patients make informed decisions and encourages early consultation with a qualified general surgeon.