Table of Contents
- Understanding Allergies, Blockages, and Dry Eye Syndrome
- When Allergies Turn the Tap On and Cause Watery Eyes
- Why Blockages Occur: A Common Cause of Watery Eyes
- How Dry Eye Triggers Excess Tearing and Watery Eyes
- When Professional Care Is Necessary
- Personalized Treatment Solutions for Lasting Watery Eye Relief
- Dr. Rachana Tiwari-Patil: A Trusted and Compassionate Eye Specialist
Why Do You Have Watery Eyes? Allergies, Blockages, and Dry Eye Explained by Expert Eye Specialist Dr. Rachana Tiwari-Patil
There is a peculiar frustration that comes with eyes that refuse to stay dry. One instant, your vision feels perfectly composed; the next, tears spill over as if summoned by an invisible switch. You dab, blink, apologize, and wonder whether onlookers assume you are quietly unraveling. In reality, persistently watery eyes are far from rare. What is uncommon is how often their root cause is misunderstood.
Excessive tearing can be traced to very different origins. Sometimes it’s an immune overreaction to harmless particles. Sometimes it’s a plumbing failure within the eye’s drainage network. And at times—most paradoxically—it is dryness itself that provokes the flood. Knowing which mechanism is at play transforms confusion into clarity and guesswork into targeted relief.
Below, we untangle the three primary offenders behind incessant tearing and outline how to distinguish one from another without relying on hunches or hearsay.
How the Inner Mechanics of Tears Cause Watery Eyes
Before isolating the cause, it helps to appreciate the quiet choreography happening within your eyes every waking moment. Tear production is not episodic; it is continuous. Lacrimal glands positioned above each eye secrete fluid designed to lubricate, cleanse, and nourish the ocular surface. These tears spread with each blink, forming a protective veil over the cornea.
Once their task is complete, tears are meant to exit discreetly. They drain through minuscule openings along the eyelids—known as puncta—then pass through slender channels before emptying into the nasal cavity. When this system hums along, you never notice it. When balance is lost, tears accumulate where they don’t belong.
Disruption can occur in three ways: excessive production, impaired drainage, or poor tear quality. Though the outcome looks identical in the mirror, the causes could not be more distinct.
When Allergies Turn the Tap On and Cause Watery Eyes
Allergic conjunctivitis remains the most frequent instigator of watery eyes. If your symptoms appear suddenly, fluctuate with the environment, or worsen during specific seasons, allergens are the likely provocateurs.
Hallmarks of Eye Allergies
Allergy-driven tearing rarely arrives alone. It travels with a recognizable entourage of symptoms:
- Intermittent yet profuse tearing
- Relentless itching that tempts constant rubbing
- Diffuse redness reminiscent of recent crying
- Puffiness, particularly along the eyelids
- Stinging or burning sensations
- Clear, thin discharge
What defines allergic reactions most clearly is their predictability. The eyes respond when exposed to specific triggers rather than at random.
Common irritants include airborne pollen, dust mites embedded in household fabrics, animal dander, mold spores in humid spaces, and even certain cosmetic products or ophthalmic solutions.
Seasonal Patterns vs. Perennial Irritants
Many individuals notice a rhythmic quality to their symptoms. Spring often ushers in tree pollen woes. Summer favors grasses. Autumn introduces ragweed. Indoor allergens, on the other hand, show no respect for calendars and can provoke symptoms year-round.
If your eyes protest more in certain locations or times of year, allergies are likely steering the reaction. Once identified, triggers can often be minimized, and symptoms managed with relative ease.
When Tear Ducts Fail to Drain
Imagine a sink with a blocked outlet. Water continues to flow, but escape is impossible. A blocked tear duct operates under the same principle. Tears are produced as usual, yet they have nowhere to go.
Clinically termed dacryostenosis, tear duct obstruction can affect individuals at any age, though it is especially prevalent among infants and older adults.
How Tear Drainage Becomes Obstructed
The tear drainage pathway is a narrow, winding route. Tears move from puncta into canaliculi, collect in a small reservoir, and then descend through the nasolacrimal duct into the nose. Obstruction at any point along this route results in overflow.
Typical indicators include:
- Constant tearing from one or both eyes
- Tears tracking down the cheek without provocation
- Sticky residue, particularly after sleep
- Discomfort or pressure near the inner eye corner
- Localized swelling
- Recurrent eye infections
Unlike allergies, tearing from a blockage tends to be steady rather than episodic.
Why Blockages Occur: A Common Cause of Watery Eyes
Several factors can constrict or seal the drainage system. Age-related tissue changes may narrow ducts. Past trauma or surgical procedures can leave behind scar tissue. Chronic sinus inflammation or nasal polyps may obstruct drainage indirectly. Certain systemic medications, including Chronic sinus inflammation or nasal polyps, may obstruct drainage indirectly. Certain systemic medications, including some chemotherapeutic agents, are also known contributors.
In newborns, blocked tear ducts are often congenital, resulting from incomplete development. Many resolve naturally within months, though persistent cases may require intervention.
The Dry Eye Paradox
Among the most counterintuitive causes of watery eyes is dry eye syndrome. Here, the eyes overflow not because they are well-lubricated, but because they are inadequately protected.
How Dry Eye Triggers Excess Tearing and Watery Eyes
Healthy tears are complex, composed of water, oils, and mucus. When this mixture is deficient—either in volume or quality—the ocular surface becomes irritated. In response, the nervous system triggers emergency tear production.
These reflex tears resemble a sudden downpour: abundant, thin, and poorly equipped to nourish or stabilize the eye. They wash over the surface briefly, then evaporate or drain away, leaving dryness unresolved.
Thus begins a maddening loop: irritation prompts tearing, tearing fails to soothe, and irritation persists.
Signs Pointing to Dry Eye Syndrome
Dry eye does not announce itself subtly. Symptoms often include:
- A gritty or sandy sensation
- Watering that worsens outdoors or in the wind
- Burning or sharp stinging
- Light sensitivity
- Contact lens intolerance
- Fluctuating or blurry vision that improves with blinking
- Visual fatigue after prolonged focus
- String-like mucus discharge
This blend of dryness and excess tearing is a defining clue.
Who Is Most at Risk
Dry eye syndrome becomes more prevalent with age as tear production naturally declines. Hormonal fluctuations—particularly in women—play a significant role. Environmental stressors such as arid air, heating systems, and persistent wind exacerbate symptoms.
Modern habits add fuel to the fire. Prolonged screen use suppresses blinking, accelerating tear evaporation. Medications like antihistamines, decongestants, and antidepressants can reduce tear output. Contact lenses may further destabilize the tear film.
Pinpointing the True Cause
Because symptoms overlap, accurate identification is essential. Small details matter. Timing, triggers, consistency, and accompanying sensations all offer diagnostic breadcrumbs.
Keeping a brief symptom log for one or two weeks can be revealing. Record when tearing occurs, what you were doing, environmental conditions, and any relief measures that helped—or failed. This record can be invaluable during a clinical evaluation.
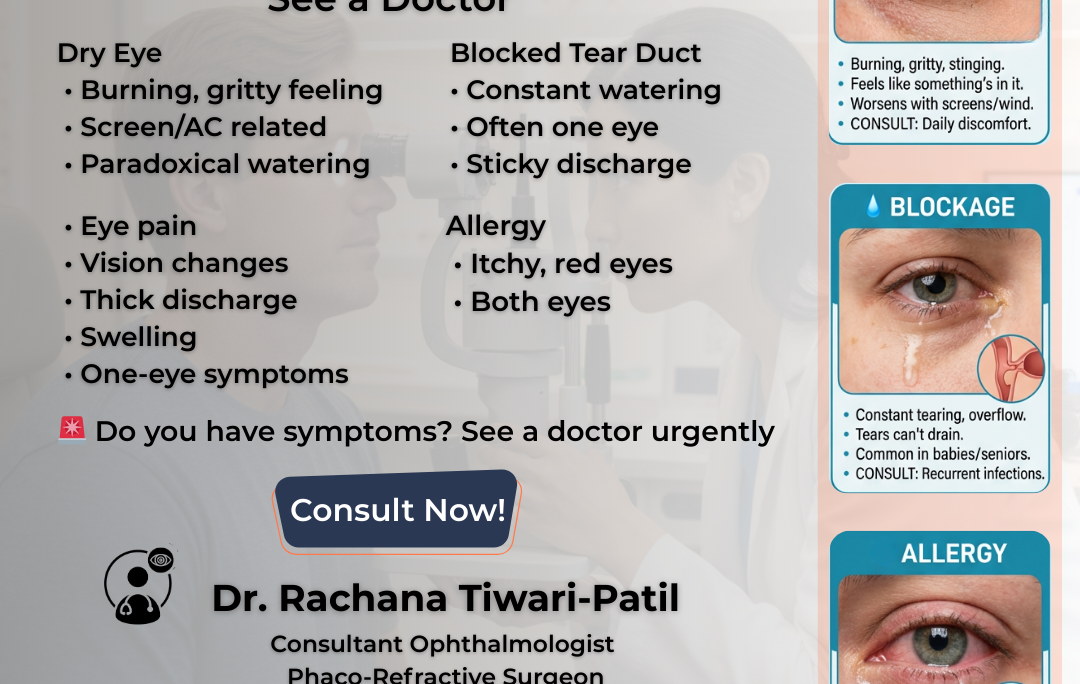
When Professional Care Is Necessary
Occasional tearing is rarely alarming. Persistent or disruptive symptoms, however, deserve medical attention. Consult an eye care professional if you notice:
- Ongoing tearing that interferes with daily tasks
- Thick yellow or green discharge
- Noticeable pain or visual changes
- Symptoms unresponsive to non-prescription treatments
Ophthalmologists and optometrists can assess tear production, inspect drainage pathways, evaluate tear quality, and test for allergens using specialized tools.
Personalized Treatment Solutions for Lasting Watery Eyes Relief
Treatment is only effective when it matches the cause.
Allergic eye conditions often respond well to trigger avoidance, antihistamine eye drops, and cooling compresses to calm inflammation.
Tear duct blockages may improve with warm compresses and massage, though persistent obstructions sometimes require minimally invasive procedures to restore proper drainage.
Dry eye management focuses on enhancing tear stability. Artificial tears, prescription therapies, and interventions that slow tear loss are common strategies. Environmental adjustments—such as humidifiers and regular screen breaks—also play a meaningful role.
Watery eyes may seem trivial, yet their impact on comfort, productivity, and confidence can be profound. Whether the culprit is allergies, obstruction, or dry eye syndrome, understanding the distinction is the gateway to relief. If symptoms linger or intensify, seeking expert care is not indulgence—it is preservation. Your eyes, after all, are not expendable instruments. They deserve informed attention and deliberate care.
Dr. Rachana Tiwari-Patil: A Trusted and Compassionate Eye Specialist
Dr. Rachana Tiwari-Patil stands as a meticulous and empathetic ophthalmologist at Chetna Hospital, where clinical rigor meets genuine human care. Her work reflects a rare equilibrium—scientific exactitude balanced with a soothing bedside presence. Patients entering her consultation room often remark on the quiet confidence with which she navigates both routine visual complaints and intricate ocular disorders.
Her expertise spans a broad ophthalmic spectrum. From persistently watering eyes and chronic dry eye syndrome to allergic inflammations and nuanced tear duct abnormalities, Dr. Tiwari-Patil approaches each case as a distinct narrative rather than a textbook repetition. She treats the eye not as an isolated organ, but as a storyteller, revealing clues about deeper physiological imbalances.
At the core of her practice lies a resolute patient-centric ethos. She listens with intent, probes with precision, and explains with clarity that never feels rushed or rehearsed. For her, diagnosis is not merely the identification of symptoms—it is an investigative journey to uncover the true origin of discomfort. This philosophy fosters trust, allowing patients to feel anchored and assured as they progress through their treatment.
Dr. Tiwari-Patil’s clinical methodology is grounded in accuracy and foresight. Each treatment plan is sculpted to the individual, factoring lifestyle, progression risk, and long-term ocular resilience. Her consultations are marked by thoughtful deliberation, an unhurried demeanor, and an ethical compass that prioritizes sustainable eye health over quick fixes.
Continuing her dedicated service at Chetna Hospital, Dr. Rachana Tiwari-Patil remains committed to enhancing visual clarity and ocular comfort. Through her discerning eye and compassionate care, she helps patients reclaim not just sharper vision, but an improved quality of life—one carefully considered diagnosis at a time.