Have you ever woken up with crusty, red eyes that feel like there’s sand in them? Or maybe you’ve noticed someone at work constantly rubbing their pink, watery eyes? Chances are, you’ve encountered conjunctivitis – commonly known as “pink eye.” This incredibly common eye condition affects millions of people every year, yet many folks don’t know how to handle it properly.
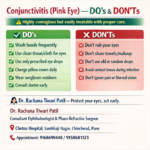
Conjunctivitis might sound scary, but it’s actually one of the most treatable eye problems out there. The key is knowing what TO do & what NOT to do when those telltale symptoms appear. Making the wrong choices can turn a minor irritation into a weeks-long ordeal, while smart decisions can have you feeling better in just a few days.
In this comprehensive guide, we’ll walk through everything you need to know about managing conjunctivitis effectively. From recognizing the FIRST signs to understanding when you absolutely must see a doctor, we’ve got you covered. We’ll also debunk some common myths that might be making your symptoms worse without you even realizing it. Whether you’re dealing with viral, bacterial, or allergic conjunctivitis, the strategies we discuss will help you navigate this frustrating condition with confidence. By the time you finish reading, you’ll be equipped with practical, easy-to-follow advice that could save you days of discomfort & prevent spreading the infection to others.
Understanding the Enemy: What Exactly IS Conjunctivitis?
Before diving into the do’s & don’ts, let’s get clear on what we’re dealing with. Conjunctivitis is inflammation of the conjunctiva – that thin, clear layer covering the white part of your eye & the inside of your eyelids. Think of it as your eye’s protective blanket getting irritated & swollen. When this happens, tiny blood vessels become more visible, giving your eyes that characteristic pink or red appearance.
There are three main types of conjunctivitis, & each requires slightly different approaches. Viral conjunctivitis is the most common type, often accompanying cold symptoms like a runny nose or sore throat. It’s HIGHLY contagious but usually clears up on its own within 7-14 days. Bacterial conjunctivitis typically produces thicker, yellowish discharge & can affect one or both eyes. This type responds well to antibiotic treatment when properly diagnosed. Allergic conjunctivitis occurs when your eyes react to allergens like pollen, pet dander, or dust mites. Unlike infectious types, allergic conjunctivitis isn’t contagious but can be incredibly frustrating to manage.
The symptoms often overlap between types, which is why many people struggle with proper treatment. Common signs include redness, itching, burning sensation, excessive tearing, & discharge that may cause your eyelids to stick together, especially after sleeping. Some people also experience sensitivity to light or a feeling like something is stuck in their eye. Understanding these differences is CRUCIAL because using the wrong treatment approach can actually make things worse or prolong your recovery time.
The Essential DO’S: Your Action Plan for Fast Recovery
When conjunctivitis strikes, your first instinct might be to rub your eyes or ignore the symptoms hoping they’ll go away. Instead, here’s what you SHOULD do to promote healing & prevent complications. Start by washing your hands frequently with soap & warm water for at least 20 seconds. This simple step is your strongest weapon against spreading the infection to your other eye or to family members.
Apply warm or cool compresses to affected eyes for 5-10 minutes several times throughout the day. Warm compresses work particularly well for bacterial conjunctivitis, helping to loosen crusty discharge & soothe irritation. Cool compresses are often more comfortable for viral or allergic types, providing relief from itching & swelling. Always use clean washcloths for each application, & don’t share compresses between eyes if only one is affected.
Keep your eyes clean by gently removing discharge with a fresh, damp cloth. Wipe from the inner corner toward the outer corner, using a different section of the cloth for each wipe. This technique prevents recontamination & helps clear away irritating substances. If you wear contact lenses, STOP wearing them immediately & switch to glasses until your symptoms completely resolve. Contacts can trap bacteria & irritants against your eye, significantly prolonging recovery time.
Replace your eye makeup, especially mascara & eyeliner, if you used them while infected. These products can harbor bacteria & reinfect your eyes even after symptoms disappear. Consider this an opportunity to try new products! Also, wash pillowcases, towels, & anything else that touched your face in hot water to eliminate lingering germs.
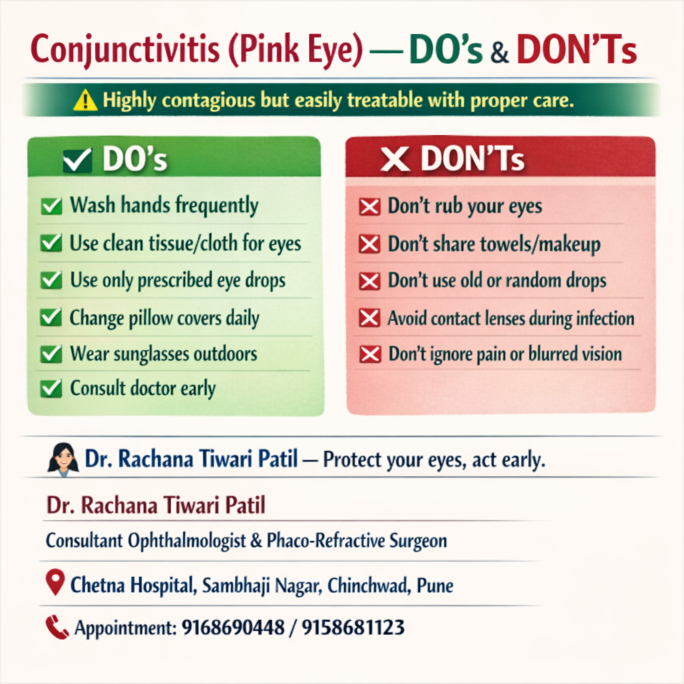
Critical DON’TS: Mistakes That Could Make Everything Worse
Now let’s talk about what NOT to do – these mistakes are surprisingly common & can turn a minor case of conjunctivitis into a major headache. Never, EVER touch or rub your infected eyes with unwashed hands. This seems obvious, but when your eyes are itchy & irritated, the urge to rub them can be overwhelming. Rubbing not only spreads infection but can also damage the delicate tissue around your eyes.
Don’t share personal items like towels, washcloths, pillowcases, or makeup with others while you’re infected. Even family members should use separate items until your symptoms are completely gone. This includes avoiding sharing drinks, especially if you’ve touched the rim with contaminated hands. Many families unknowingly pass conjunctivitis back & forth because they don’t realize how easily it spreads through shared objects.
Avoid swimming in pools, hot tubs, or natural bodies of water while infected. Chlorinated water can irritate already sensitive eyes, while lakes & rivers may contain additional bacteria that could worsen your condition. Plus, you risk spreading your infection to other swimmers. Most public pools actually require people with conjunctivitis to stay out until they’re no longer contagious.
Don’t use over-the-counter eye drops without consulting a healthcare provider first. While some artificial tears can provide relief, medicated drops might not be appropriate for your specific type of conjunctivitis. Using the wrong drops could mask symptoms, making it harder to determine if you need prescription treatment. Additionally, some drops contain preservatives that can further irritate sensitive eyes.
When to Seek Professional Help: Red Flags You Shouldn’t Ignore
While many cases of conjunctivitis resolve on their own, certain situations require immediate medical attention. Don’t play the waiting game if you experience severe eye pain, significant vision changes, or extreme sensitivity to light. These symptoms could indicate a more serious condition that requires prompt treatment to prevent permanent damage.
Seek medical care if your symptoms worsen after 2-3 days of home treatment or don’t improve within a week. Bacterial conjunctivitis often requires antibiotic drops or ointments to clear completely, & delaying treatment can lead to complications. If you notice thick, colored discharge (especially green or yellow), this typically signals bacterial infection requiring prescription medication.
People with compromised immune systems, contact lens wearers, & those with underlying eye conditions should see a healthcare provider sooner rather than later. These groups face higher risks of complications & may need specialized treatment approaches. Newborns & infants with any signs of conjunctivitis need immediate medical evaluation, as their developing immune systems can’t fight infections as effectively as adults.
If you develop fever, swollen lymph nodes, or other systemic symptoms alongside your eye problems, this could indicate a more serious infection spreading beyond your eyes. Don’t hesitate to contact your healthcare provider or visit an urgent care center if you’re concerned about your symptoms.
Your Path to Clear, Healthy Eyes
Managing conjunctivitis doesn’t have to be complicated or stressful when you know the right steps to take. Remember that the vast majority of cases resolve completely with proper care & attention to hygiene. The KEY is acting quickly, following appropriate treatment guidelines, & knowing when professional help is necessary.
Prevention remains your best strategy for avoiding future episodes. Wash your hands regularly, avoid touching your eyes, & don’t share personal items that come into contact with your face. If you’re prone to allergic conjunctivitis, work with your doctor to identify triggers & develop a management plan before symptoms start.
Most importantly, don’t let embarrassment or inconvenience prevent you from seeking help when you need it. Conjunctivitis is incredibly common, & healthcare providers see cases every single day. Early intervention can save you weeks of discomfort & prevent the infection from spreading to others in your household or workplace.
Take charge of your eye health by implementing these strategies the moment symptoms appear. Your future self will thank you for taking decisive action instead of hoping the problem will magically disappear. Clear, comfortable vision is worth the effort, & with the right approach, you’ll be back to normal activities before you know it. Keep this guide handy, share it with family members, & remember – when it comes to your eyes, it’s always better to be safe than sorry.