Shoulder pain can turn simple tasks like reaching for a coffee mug or getting dressed into painful ordeals. This guide is for anyone dealing with shoulder discomfort—whether you’re an athlete with a sports injury, an office worker with repetitive strain, or someone experiencing sudden pain without knowing why.
Finding the right shoulder pain treatment doesn’t have to be overwhelming. We’ll walk you through identifying what’s causing your pain and when you should see a doctor right away. You’ll also discover immediate relief techniques you can try at home, plus learn about professional treatment options that can get you back to your normal activities faster.
Identify Common Causes of Shoulder Pain
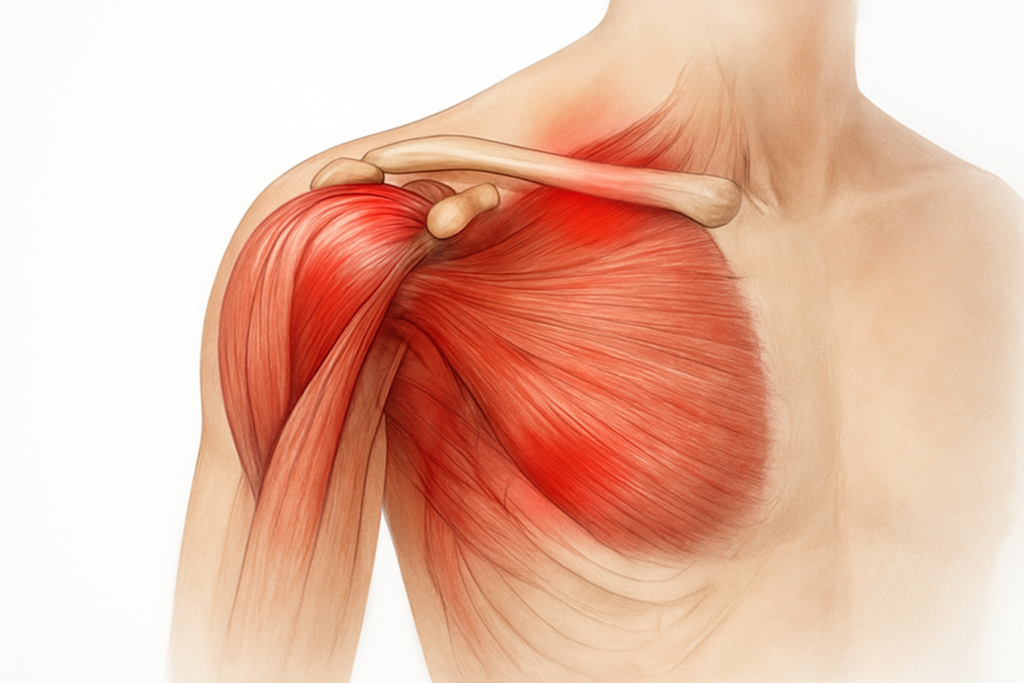
Rotator Cuff Injuries and Tears
The rotator cuff stands as one of the most vulnerable areas when we talk about shoulder pain. This complex network of four muscles and tendons wraps around your shoulder joint like a protective sleeve, keeping your upper arm bone securely in place while allowing for that impressive range of motion we often take for granted.
Rotator cuff injuries happen more often than you might think. Athletes who repeatedly throw or lift overhead – think baseball pitchers, swimmers, or tennis players – put enormous stress on these tissues. But here’s the surprising part: you don’t need to be an athlete to experience this type of injury. Simple activities like reaching for items on high shelves, painting a ceiling, or even sleeping on your side wrong can trigger problems.
The injury typically develops in two ways. Acute tears occur suddenly, often from a fall on an outstretched arm or lifting something too heavy with poor form. You’ll know this has happened because the pain hits like lightning, accompanied by immediate weakness and difficulty moving your arm. Chronic tears, on the other hand, develop slowly over months or years. These sneaky injuries result from repetitive stress and gradual wear-and-tear, making them harder to pinpoint initially.
Age plays a significant role in rotator cuff problems. After 40, these tendons begin losing their natural elasticity and blood supply decreases, making them more susceptible to injury. The tendons literally start fraying like old rope, which explains why rotator cuff tears become increasingly common as we age.
The symptoms vary depending on the severity of the injury. Partial tears might cause a dull ache that worsens at night, especially when lying on the affected side. Complete tears often produce sharp, intense pain accompanied by significant weakness – you might find yourself unable to lift your arm away from your body or reach behind your back.
Treatment approaches range from conservative management to surgical intervention. Small tears often respond well to rest, ice, and physical therapy focusing on strengthening the surrounding muscles. Larger tears or those causing persistent weakness may require arthroscopic repair or, in severe cases, open surgery.
Frozen Shoulder and Adhesive Capsulitis
Frozen shoulder, medically known as adhesive capsulitis, represents one of the most frustrating shoulder conditions because it literally locks up your joint. The shoulder capsule – a strong connective tissue that surrounds the joint – becomes thick, tight, and inflamed, creating adhesions that severely restrict movement.
This condition affects roughly 2-5% of the population, with women between ages 40-60 being particularly susceptible. The exact cause remains somewhat mysterious, but certain factors increase your risk significantly. Diabetes tops the list, with diabetic individuals being 2-4 times more likely to develop frozen shoulder. Other conditions like thyroid disorders, cardiovascular disease, and Parkinson’s disease also elevate risk levels.
Frozen shoulder progresses through three distinct stages, each lasting several months. The freezing stage brings gradually increasing pain and stiffness. Sleep becomes difficult as pain intensifies at night, and simple activities like combing your hair or reaching into a back pocket become challenging or impossible.
The frozen stage follows, where pain may actually decrease, but stiffness reaches its peak. Your shoulder feels locked in place, with severely limited range of motion in all directions. This stage can be particularly depressing because while the constant pain subsides, the functional limitations feel overwhelming.
Finally, the thawing stage brings gradual improvement. Range of motion slowly returns over many months, though some people never regain complete mobility. The entire process typically takes 1-3 years, which explains why frozen shoulder tests patience like few other conditions.
Treatment focuses on pain management and preserving whatever range of motion remains. Anti-inflammatory medications help control pain and inflammation during the acute phase. Physical therapy becomes crucial, though it must be approached carefully to avoid aggravating the condition. Gentle stretching and range-of-motion exercises help prevent further stiffening.
For severe cases, doctors might recommend corticosteroid injections to reduce inflammation, or in rare instances, manipulation under anesthesia or arthroscopic capsular release to break up adhesions.
Arthritis and Joint Degeneration
Shoulder arthritis affects millions of people worldwide, causing pain, stiffness, and decreased mobility that significantly impacts daily life. Unlike other forms of shoulder pain that might develop suddenly, arthritis typically develops gradually as joint cartilage wears away over time.
Osteoarthritis, the most common type affecting shoulders, results from years of wear and tear on the joint surfaces. The smooth cartilage that normally allows bones to glide effortlessly against each other begins to break down, creating rough, irregular surfaces that grind together painfully. This process accelerates after age 50, though it can begin earlier in people with previous injuries or genetic predisposition.
Rheumatoid arthritis presents a different challenge. This autoimmune condition causes the body’s immune system to attack joint tissues, leading to inflammation, pain, and eventual joint destruction. Unlike osteoarthritis, rheumatoid arthritis often affects multiple joints simultaneously and can strike at any age.
Post-traumatic arthritis develops following significant shoulder injuries. Fractures, dislocations, or severe soft tissue injuries can damage cartilage or alter joint mechanics, accelerating the degenerative process. Athletes with histories of shoulder injuries often face this type of arthritis years after their playing careers end.
The symptoms of shoulder arthritis develop gradually. Early stages might bring only occasional stiffness or mild pain after activity. As the condition progresses, pain becomes more constant and severe, often described as a deep aching sensation. Morning stiffness lasting more than 30 minutes becomes common, and range of motion decreases noticeably.
Night pain frequently disrupts sleep, particularly when lying on the affected side. You might notice grinding or catching sensations during movement, along with weakness that makes lifting objects or reaching overhead increasingly difficult.
Non-surgical treatments form the foundation of arthritis management. Anti-inflammatory medications help control pain and swelling, while preserving joint function through appropriate activity modification. Physical therapy emphasizes maintaining range of motion and strengthening surrounding muscles to support the affected joint.
Heat and cold therapy can provide significant relief. Warm showers or heating pads help reduce stiffness, while ice packs can decrease inflammation after activity. Many people find alternating between heat and cold particularly beneficial.
When conservative treatments fail to provide adequate relief, surgical options include arthroscopic debridement to clean out loose cartilage fragments, or shoulder replacement surgery for severe cases.
Muscle Strains and Overuse Injuries
Muscle strains and overuse injuries represent some of the most common yet preventable causes of shoulder pain. These injuries develop when muscles, tendons, or ligaments are stretched beyond their normal capacity or subjected to repetitive stress without adequate recovery time.
Acute muscle strains often occur during sudden, forceful movements or when muscles are stretched while contracting. Picture reaching aggressively for a tennis serve or lifting a heavy box with poor form – these scenarios frequently result in immediate muscle fiber tearing and subsequent pain.
Overuse injuries develop more insidiously through repetitive motions performed over extended periods. Office workers who spend hours at computers with poor ergonomics, factory workers performing repetitive assembly tasks, or weekend warriors who suddenly increase their activity level without proper conditioning all face elevated risks.
The deltoid muscle, which caps your shoulder, commonly experiences strains from overhead activities. Pain typically localizes to the outer shoulder and worsens with arm elevation. Simple tasks like putting on a shirt or reaching for objects become uncomfortable.
The trapezius muscle, extending from your neck to your shoulder blade, frequently develops trigger points and tension from poor posture or stress. This creates referred pain patterns that can confuse diagnosis, as pain might appear in the neck, shoulder, or even down the arm.
Bicep strains affect the long head of the biceps tendon as it passes through the shoulder joint. This injury often produces pain in the front of the shoulder that worsens with overhead movements or when trying to lift objects.
Early recognition of overuse injuries can prevent minor problems from becoming major limitations. Initial symptoms often include mild soreness after activity that resolves with rest. As the condition progresses, pain becomes more persistent and may interfere with daily activities.
Treatment for muscle strains depends on severity. Grade 1 strains involve microscopic muscle fiber damage and typically heal within a few days with rest, ice, and gentle stretching. Grade 2 strains involve partial muscle tears and may require 2-6 weeks of modified activity and physical therapy. Grade 3 strains represent complete muscle tears that might need surgical repair.
The RICE protocol (Rest, Ice, Compression, Elevation) provides immediate relief for acute strains. Anti-inflammatory medications help control pain and swelling during the first few days. As pain subsides, gentle range-of-motion exercises prevent stiffness, followed by gradual strengthening as healing progresses.
Prevention strategies focus on proper warm-up before activities, maintaining good posture during work, and gradually increasing activity levels rather than jumping into intense exercise after prolonged inactivity. Ergonomic workplace adjustments and regular stretching breaks can significantly reduce overuse injury risk.
Understanding these common causes of shoulder pain empowers you to seek appropriate shoulder pain treatment early, potentially preventing minor issues from developing into chronic problems that significantly impact your quality of life.
Recognize Warning Signs That Require Immediate Medical Attention

Sudden Severe Pain After Trauma
When shoulder pain strikes suddenly after an injury or trauma, your body is sending a clear distress signal that demands immediate attention. This type of pain differs dramatically from the gradual ache you might experience from overuse or poor posture. Traumatic shoulder injuries can involve complex structures including bones, ligaments, tendons, and surrounding muscles, making quick medical evaluation critical for proper shoulder pain treatment.
Sudden severe pain typically manifests as an intense, sharp sensation that may radiate down your arm or up into your neck. The pain often feels different from anything you’ve experienced before – it’s the kind that makes you stop whatever you’re doing and clutch your shoulder involuntarily. This isn’t the dull throb you can push through; it’s debilitating and overwhelming.
Several serious conditions can cause this type of immediate, severe pain. A shoulder dislocation represents one of the most common traumatic injuries, occurring when the upper arm bone pops out of the shoulder socket. This creates intense pain accompanied by visible deformity of the shoulder area. The shoulder may appear “squared off” rather than rounded, and you’ll likely be unable to move your arm at all.
Fractures of the shoulder bones, including the humerus (upper arm bone), clavicle (collarbone), or scapula (shoulder blade), also produce severe immediate pain. These injuries often result from high-impact trauma like car accidents, falls from significant heights, or direct blows during contact sports. The pain from a fracture is typically constant and worsens with any attempt at movement.
Rotator cuff tears, particularly complete tears, can cause sudden severe pain, especially if they occur during a traumatic event. While some rotator cuff injuries develop gradually, traumatic tears produce immediate, intense pain that may extend down your arm. You might hear or feel a “pop” at the moment of injury, followed by immediate weakness and pain.
Acromioclavicular (AC) joint separations represent another serious injury causing sudden severe pain. These occur when the ligaments connecting your collarbone to your shoulder blade tear, often from falls onto the shoulder or direct impacts. The pain is typically localized to the top of the shoulder and may be accompanied by visible swelling or deformity.
The timing of medical intervention directly impacts treatment outcomes for traumatic shoulder injuries. Dislocations, for instance, become more difficult to reduce (put back in place) as time passes and swelling increases. Fractures require prompt stabilization to prevent further damage to surrounding soft tissues, blood vessels, and nerves. Delaying treatment can lead to complications including chronic pain, reduced range of motion, and increased risk of future injuries.
When severe pain follows trauma, don’t attempt to “tough it out” or wait to see if it improves. Your shoulder’s complex anatomy means that seemingly minor injuries can mask more serious underlying damage. Professional medical evaluation within hours of injury provides the best opportunity for optimal recovery and prevents long-term complications that could affect your quality of life.
Complete Loss of Shoulder Movement
Complete inability to move your shoulder represents a medical emergency that requires immediate professional evaluation. This condition, known medically as shoulder immobility or “frozen” shoulder in acute cases, differs from simple stiffness or reluctance to move due to pain. True complete loss of movement means you cannot lift, rotate, or move your arm in any direction, regardless of your effort or pain tolerance.
Several serious conditions can cause complete loss of shoulder movement. Shoulder dislocations frequently result in complete immobility as the displaced bone prevents normal joint function. The muscles surrounding the joint may also go into protective spasm, further limiting any possible movement. Even if you try to move your arm with your other hand, the shoulder joint won’t respond normally.
Severe fractures, particularly those involving the shoulder joint itself, can mechanically prevent movement. When bone fragments shift or when the fracture disrupts the smooth joint surfaces, normal mechanics become impossible. These injuries often occur from high-energy trauma and may involve multiple bone fragments that physically block joint motion.
Complete rotator cuff tears, especially massive tears involving multiple tendons, can result in loss of active shoulder movement. While the joint itself may not be mechanically blocked, the muscles responsible for moving your arm become non-functional. You might retain some passive range of motion (someone else can move your arm), but you cannot actively lift or rotate your arm on your own.
Nerve injuries represent another serious cause of complete shoulder immobility. The brachial plexus, a network of nerves controlling shoulder and arm function, can be damaged in severe trauma. When these nerves are injured, the muscles they control become paralyzed, resulting in complete loss of voluntary movement. This type of injury often accompanies motorcycle accidents, severe falls, or other high-impact traumas.
Severe infections within the shoulder joint, though less common, can also cause complete loss of movement. These infections, called septic arthritis, create intense pain and swelling that makes any movement impossible. The joint may feel hot and swollen, and you’ll likely have fever and other signs of systemic illness.
The inability to move your shoulder completely represents a orthopedic emergency requiring immediate medical attention. Quick diagnosis and treatment can prevent permanent damage to joints, muscles, and nerves. Delayed treatment may result in chronic disability, persistent pain, and long-term functional limitations that significantly impact daily activities.
Time-sensitive injuries like dislocations have optimal outcomes when treated within hours of occurrence. As swelling increases and muscles tighten, reduction becomes more difficult and may require surgical intervention instead of simpler closed reduction techniques. Fractures with complete loss of movement often indicate displaced or unstable breaks that require prompt surgical stabilization to prevent permanent joint damage.
Numbness or Tingling in the Arm
Numbness or tingling in your arm accompanying shoulder pain represents a serious warning sign that nerve structures may be compressed, damaged, or compromised. These neurological symptoms, medically termed paresthesias, indicate that the problem extends beyond simple muscle or joint issues and involves the complex nerve pathways that control sensation and movement in your arm and hand.
The sensation of numbness typically feels like your arm has “fallen asleep” but doesn’t resolve with changing positions or shaking your arm. You might experience reduced ability to feel touch, temperature, or pressure in specific areas of your arm, hand, or fingers. Tingling often accompanies numbness and may feel like pins and needles, electrical sensations, or burning feelings that travel down your arm.
These symptoms can result from several serious conditions requiring immediate medical evaluation. Cervical radiculopathy occurs when nerve roots exiting the cervical spine become compressed or irritated. While the problem originates in your neck, the symptoms often present as shoulder pain accompanied by numbness and tingling that follows specific nerve pathways down your arm. Different nerve roots produce characteristic patterns of numbness and tingling in predictable areas of your arm and hand.
Thoracic outlet syndrome represents another serious condition where nerves and blood vessels become compressed as they travel between your neck and armpit. This compression can occur at several anatomical locations, creating numbness and tingling in your arm, hand, and fingers. The symptoms often worsen with certain arm positions or activities that further narrow the space where nerves travel.
Brachial plexus injuries, whether from trauma or other causes, can produce numbness and tingling throughout your arm. The brachial plexus consists of nerve roots from your neck that combine and separate to form the nerves controlling your shoulder, arm, and hand. Damage to any part of this complex network can create numbness, tingling, weakness, or complete loss of sensation in specific patterns depending on which nerves are affected.
Peripheral nerve compression can also cause these symptoms. The median nerve, which travels through your arm to your hand, can become compressed at various points along its path. While carpal tunnel syndrome is the most well-known compression site, the nerve can also be compressed higher up in your arm or shoulder area, creating numbness and tingling that might be mistakenly attributed to shoulder problems alone.
Circulatory problems affecting blood flow to your arm can also produce numbness and tingling. Blood clots, arterial compression, or other vascular issues can reduce circulation to your arm, creating symptoms similar to nerve compression. These conditions require immediate medical attention to prevent permanent tissue damage.
The pattern and distribution of numbness and tingling provide crucial diagnostic information. Different nerves control sensation in specific areas of your arm and hand, so mapping where you experience these symptoms helps medical professionals identify which structures are involved. Keeping track of exactly where you feel numbness or tingling, when symptoms worsen or improve, and what activities trigger them provides valuable information for proper diagnosis.
Timing becomes critical when numbness and tingling accompany shoulder pain. Nerve compression or damage can become permanent if not addressed promptly. Early intervention often provides the best outcomes for nerve-related problems, while delayed treatment may result in chronic numbness, weakness, or pain that significantly impacts your daily function and quality of life.
Progressive worsening of numbness and tingling symptoms represents a particular concern. If you notice that the affected area is expanding, symptoms are becoming more intense, or you’re developing weakness along with the sensory changes, seek immediate medical attention. These signs may indicate that nerve compression or damage is worsening and requires urgent intervention to prevent permanent injury.
The combination of shoulder pain with arm numbness and tingling should never be ignored or attributed to simple muscle strain. These symptoms indicate involvement of your nervous system and require professional medical evaluation to determine the underlying cause and appropriate shoulder pain treatment approach.
Apply Immediate Relief Techniques for Acute Pain
Ice Therapy for First 48 Hours
When shoulder pain strikes suddenly, ice becomes your first line of defense. The cold temperature works by numbing the area and reducing inflammation at the cellular level. Blood vessels constrict when exposed to cold, which limits the flow of inflammatory substances to the injured tissues. This process, called vasoconstriction, helps prevent excessive swelling that can worsen pain and delay healing.
Apply ice for 15-20 minutes at a time, several times throughout the day during the first 48 hours after injury. Never place ice directly on your skin – always wrap it in a thin towel or cloth to prevent frostbite. A bag of frozen peas works just as well as traditional ice packs and molds better to the shoulder’s contours.
The timing matters more than you might think. Starting ice therapy within the first few hours after injury maximizes its effectiveness. After 48 hours, the acute inflammatory phase typically subsides, and continued ice therapy may actually slow down the healing process by restricting blood flow that brings healing nutrients to the area.
Some people find contrast therapy helpful after the initial 48-hour period. This involves alternating between ice (10 minutes) and heat (10 minutes) to promote blood flow while still controlling inflammation. However, stick to ice-only during those crucial first two days.
Watch for signs that you’re overdoing the ice therapy. If your skin becomes red, numb, or develops a burning sensation, remove the ice immediately. People with certain conditions like diabetes or circulation problems should be extra cautious and consult their healthcare provider before using ice therapy extensively.
Gentle Range of Motion Exercises
Movement might seem counterintuitive when your shoulder hurts, but gentle range of motion exercises prevent stiffness and maintain joint mobility. The key word here is “gentle” – you’re not trying to push through severe pain or force movement that causes sharp, shooting sensations.
Pendulum swings represent the gentlest starting point. Lean forward slightly and let your affected arm hang loosely at your side. Using your body’s movement rather than your shoulder muscles, create small circular motions with your arm. Start with tiny circles and gradually increase the size as comfort allows. This exercise uses gravity to gently mobilize the shoulder joint without putting stress on injured structures.
Wall walks help restore forward flexion gradually. Stand facing a wall with your fingertips touching it. Slowly “walk” your fingers up the wall, letting your shoulder blade glide naturally. Only go as high as comfortable – forcing the movement can cause more harm than good. Mark your progress on the wall with a piece of tape to track improvement over time.
Cross-body stretches target the posterior capsule of the shoulder. Gently pull your affected arm across your chest using your other hand. Hold for 15-30 seconds without forcing the stretch. This movement helps maintain flexibility in the back of the shoulder joint.
External rotation exercises can begin once acute pain subsides. Keep your elbow tucked against your side and slowly rotate your forearm away from your body. You can use a resistance band for very light resistance, but bodyweight alone often provides enough challenge initially.
Start these exercises 2-3 times daily, performing each movement 5-10 times. Listen to your body’s signals – some discomfort is normal, but sharp pain means you should stop immediately. The goal is maintaining movement, not pushing through significant pain barriers.
Remember that everyone’s recovery timeline differs. Some people can begin gentle exercises within 24-48 hours, while others need several days of rest first. Age, fitness level, and the type of injury all influence how quickly you can safely introduce movement.
Over-the-Counter Pain Medications
Over-the-counter medications play a valuable role in shoulder pain treatment by managing both pain and inflammation. Understanding how different medications work helps you make informed choices about what might work best for your specific situation.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and aspirin tackle both pain and inflammation simultaneously. These medications block enzymes called COX-1 and COX-2, which produce prostaglandins – chemicals that trigger inflammation and pain signals. For shoulder injuries involving tissue damage and inflammation, NSAIDs often provide more comprehensive relief than pain-only medications.
Ibuprofen typically works for 4-6 hours and comes in 200mg over-the-counter tablets. Adults can safely take 400-800mg every 6-8 hours, not exceeding 3200mg in 24 hours. Naproxen lasts longer – about 8-12 hours – making it convenient for overnight pain relief. The standard dose is 220mg every 8-12 hours.
Acetaminophen works differently by blocking pain signals in the brain rather than addressing inflammation at the injury site. While it won’t reduce swelling, it effectively manages pain and has fewer gastrointestinal side effects than NSAIDs. Adults can take 325-1000mg every 4-6 hours, with a maximum daily dose of 4000mg.
Topical preparations offer another option for localized relief. Creams or gels containing menthol, capsaicin, or topical NSAIDs like diclofenac can provide pain relief with minimal systemic absorption. These work especially well for people who can’t tolerate oral medications due to stomach sensitivity.
Timing your medication matters for optimal effectiveness. Taking NSAIDs with food reduces stomach irritation, while taking them consistently around the clock maintains steady blood levels for better inflammation control. Don’t wait until pain becomes severe – staying ahead of the pain curve works better than playing catch-up.
Safety considerations shouldn’t be overlooked, even with over-the-counter options. NSAIDs can cause stomach bleeding, kidney problems, and cardiovascular issues with long-term use. People with ulcers, kidney disease, heart problems, or those taking blood thinners should consult their healthcare provider before using NSAIDs regularly.
Acetaminophen is generally safer but can cause liver damage in high doses, especially when combined with alcohol. Read labels carefully – many cold medications and prescription pain relievers contain acetaminophen, making accidental overdose possible.
Consider alternating different types of pain relievers if single medications aren’t providing adequate relief. Some people find alternating acetaminophen and ibuprofen every 3 hours provides better pain control than either medication alone.
Proper Rest and Activity Modification
Rest doesn’t mean complete immobilization – it means modifying activities to avoid movements that aggravate your shoulder while maintaining normal daily function as much as possible. Smart activity modification promotes healing while preventing the complications that come with prolonged inactivity.
Sleep positioning significantly impacts shoulder pain recovery. Sleeping on the affected shoulder often worsens pain and interferes with healing. Try sleeping on your back with a pillow under your affected arm for support. If you’re a side sleeper, lie on your unaffected side with a pillow between your arms to prevent the injured shoulder from collapsing inward.
Some people benefit from sleeping in a recliner chair during acute phases, as the upright position reduces pressure on the shoulder joint. A wedge pillow can create a similar effect in bed by elevating your upper body at a 30-45 degree angle.
Work modifications depend on your job demands but generally involve avoiding overhead reaching, heavy lifting, and repetitive motions. Computer workers should ensure their workspace ergonomics don’t require reaching or stretching to access the keyboard or mouse. Adjust chair height and monitor position to maintain neutral shoulder positioning.
Driving considerations become important with shoulder injuries. Reaching for the steering wheel, gear shift, or seat belt can trigger pain. Adjust your seat closer to the steering wheel and use seat belt padding to reduce pressure on the shoulder. Consider avoiding highway driving during acute pain phases, as quick steering movements for lane changes can be problematic.
Household activity modifications help prevent re-injury while maintaining independence. Use your unaffected arm for reaching into cabinets, carrying groceries, and lifting objects. Store frequently used items at waist level to avoid overhead reaching. Consider using adaptive tools like reachers or grabbers for items beyond comfortable reach.
Exercise and recreational activities require careful consideration. Avoid sports involving throwing, swimming, tennis, or golf until pain subsides and range of motion returns. Walking, stationary cycling, and lower body exercises can usually continue safely. Yoga and stretching should focus on unaffected areas while avoiding poses that stress the shoulder.
The concept of “relative rest” means staying active within pain limits rather than complete bed rest. Complete immobilization can lead to muscle atrophy, joint stiffness, and decreased circulation that actually slows healing. Light activities that don’t aggravate symptoms help maintain overall fitness and prevent secondary problems.
Gradual activity progression should follow a structured approach. Start with basic daily activities like brushing teeth and combing hair. Progress to light household tasks, then gradually reintroduce work and recreational activities as symptoms improve. Setbacks are normal – if pain increases, scale back activities temporarily rather than pushing through.
Monitor your symptoms throughout the day and adjust activities accordingly. Morning stiffness might require gentle warm-up movements before starting daily activities. Afternoon fatigue might signal the need for activity modification or rest breaks.
Workplace ergonomics deserve special attention for office workers. Position your computer screen at eye level to prevent forward head posture that can stress the shoulder. Use a document holder to avoid neck rotation. Consider voice recognition software if typing aggravates symptoms.
Creating a healing environment at home involves removing obstacles that require awkward reaching or lifting. Prepare meals that don’t require extensive chopping or stirring. Stock up on easy-to-open containers and consider meal delivery services during the acute phase.
The balance between rest and activity requires constant adjustment based on your body’s signals. Too much activity delays healing, while too little activity creates new problems. Success comes from finding that sweet spot where you maintain function without aggravating symptoms.
Implement Professional Treatment Options
Physical Therapy and Rehabilitation Programs
Physical therapy stands as one of the most effective shoulder pain treatment approaches for restoring function and reducing discomfort. A skilled physical therapist can evaluate your specific condition and design a personalized program that targets your unique needs and limitations.
The initial assessment typically involves testing your range of motion, strength levels, and identifying movement patterns that trigger pain. Your therapist will examine how you perform daily activities like reaching overhead, lifting objects, or even simple tasks like combing your hair. This comprehensive evaluation helps create a roadmap for your recovery.
Manual Therapy Techniques
Physical therapists employ various hands-on techniques to improve shoulder mobility and reduce pain. Joint mobilization involves gentle movements applied to the shoulder joint to restore normal movement patterns. These techniques can help break up scar tissue and improve the gliding motion between joint surfaces.
Soft tissue mobilization targets muscles, tendons, and ligaments surrounding the shoulder. Your therapist may use techniques like myofascial release to address tight areas and trigger points that contribute to your pain. These manual approaches often provide immediate relief and set the stage for more active treatments.
Therapeutic Exercises
A well-designed exercise program forms the cornerstone of shoulder rehabilitation. Your therapist will introduce exercises gradually, starting with gentle range-of-motion movements and progressing to strength training as your condition improves.
Pendulum exercises often serve as starting points for acute shoulder pain. These involve letting your arm hang loosely and creating small circular motions, using gravity to gently move the joint without forcing it. As healing progresses, you’ll advance to active-assisted exercises where you use your good arm or equipment to help move the affected shoulder.
Resistance training becomes important once acute pain subsides. Therabands and light weights help rebuild strength in the rotator cuff muscles, deltoids, and supporting muscle groups. Your therapist will teach you proper form to prevent re-injury while maximizing benefit.
Specialized Equipment and Modalities
Modern physical therapy clinics offer various tools to enhance your recovery. Ultrasound therapy uses sound waves to promote healing in deep tissues and can help reduce inflammation. Electrical stimulation may be applied to manage pain and promote muscle activation when weakness is present.
Cold laser therapy has gained popularity as a non-invasive treatment option. This technology uses specific wavelengths of light to stimulate cellular repair and reduce inflammation at the injury site.
Home Exercise Programs
Your therapist will develop a home program that complements your in-clinic sessions. These exercises ensure continuous progress between appointments and help you take an active role in your recovery. Starting with simple stretches and gradually adding strengthening exercises, your home program becomes a vital component of long-term success.
Regular practice of prescribed exercises at home can significantly accelerate your recovery timeline. Your therapist will provide detailed instructions and may use video demonstrations to ensure you perform exercises correctly when unsupervised.
Corticosteroid Injections for Inflammation
When conservative treatments don’t provide adequate relief, corticosteroid injections offer a powerful anti-inflammatory option for shoulder pain treatment. These injections deliver medication directly to the affected area, providing targeted relief that oral medications often cannot match.
Types of Shoulder Injections
Several injection approaches exist depending on your specific condition. Subacromial injections target the space above the rotator cuff tendons and are commonly used for impingement syndrome and bursitis. The medication reduces inflammation in this crowded space, allowing tendons to move more freely.
Intra-articular injections place corticosteroids directly into the shoulder joint itself. This approach works well for arthritis, frozen shoulder, and other conditions affecting the joint surfaces. The medication can provide significant pain relief and improved mobility for several months.
Trigger point injections focus on specific muscle knots or areas of extreme tenderness. These smaller-volume injections can address localized pain sources and muscle tension that contribute to your overall discomfort.
The Injection Process
Your doctor will typically perform these injections in an office setting using sterile technique. After cleaning the injection site, they may use a local anesthetic to numb the skin. Some physicians use ultrasound guidance to ensure precise needle placement, especially for deeper structures.
The procedure itself usually takes just a few minutes. You might feel pressure or mild discomfort during the injection, but most patients find the process quite tolerable. Some people experience temporary pain relief immediately due to the local anesthetic, while others notice gradual improvement over the following days.
Expected Outcomes and Timeline
Corticosteroid injections don’t work instantly for everyone. While some people experience relief within 24-48 hours, full benefits often develop over one to two weeks. The anti-inflammatory effects can last anywhere from several weeks to several months, depending on your condition and how your body responds to the medication.
Pain relief from these injections often creates a window of opportunity for physical therapy and other treatments to be more effective. With reduced inflammation and pain, you can often participate more fully in rehabilitation exercises that might have been too uncomfortable before the injection.
Potential Side Effects and Considerations
Like any medical treatment, corticosteroid injections carry some risks. Common side effects include temporary pain increase at the injection site, which usually resolves within a day or two. Some people experience mild swelling or bruising around the injection area.
More significant but rare complications can include infection, nerve damage, or weakening of tendons with repeated injections. Your doctor will discuss these risks and help you weigh them against potential benefits based on your specific situation.
Diabetic patients should monitor blood sugar levels closely after steroid injections, as the medication can cause temporary increases in glucose levels. People with certain medical conditions or those taking specific medications may not be good candidates for these injections.
Frequency and Long-term Considerations
Most healthcare providers recommend limiting steroid injections to three or four per year in the same location. Frequent injections can potentially weaken tendons and other soft tissues over time. Your doctor will work with you to space injections appropriately while exploring other treatment options.
These injections work best as part of a comprehensive treatment plan rather than a standalone solution. Combining injections with physical therapy, activity modification, and other treatments often produces the best long-term outcomes.
Prescription Medications for Chronic Pain
When shoulder pain persists despite other interventions, prescription medications can provide significant relief and improve your quality of life. Various classes of medications target different aspects of chronic pain, from inflammation to nerve sensitization.
Anti-inflammatory Medications
Prescription-strength NSAIDs offer more potent anti-inflammatory effects than over-the-counter options. Medications like naproxen, diclofenac, and celecoxib can provide superior pain relief for inflammatory conditions affecting the shoulder.
These medications work by blocking enzymes that produce inflammatory chemicals in your body. By reducing inflammation at the source, they can address both pain and swelling that contribute to your discomfort.
Your doctor may prescribe topical anti-inflammatory gels or patches for localized application. These formulations can provide targeted relief with fewer systemic side effects compared to oral medications. Topical options work particularly well for superficial sources of pain like tendinitis or bursitis.
Muscle Relaxants
Chronic shoulder pain often involves muscle tension and spasms that perpetuate the pain cycle. Muscle relaxants like cyclobenzaprine, methocarbamol, or tizanidine can help break this cycle by reducing muscle tension and associated discomfort.
These medications work on the central nervous system to reduce muscle contractions and spasms. Many people find they sleep better when muscle tension decreases, which can contribute to overall pain improvement since poor sleep often worsens chronic pain conditions.
Some muscle relaxants also have mild anti-anxiety effects, which can be beneficial since chronic pain often creates stress and tension that worsen symptoms. Your doctor will choose specific medications based on your symptoms and medical history.
Neuropathic Pain Medications
When shoulder pain involves nerve irritation or damage, specialized medications can provide relief that traditional painkillers cannot offer. Gabapentin and pregabalin are commonly prescribed for nerve-related pain and work by calming overactive nerve signals.
These medications can be particularly helpful for conditions like thoracic outlet syndrome or when nerve compression contributes to your shoulder pain. They often start at low doses and are gradually increased to find the right balance between pain relief and side effects.
Tricyclic antidepressants like amitriptyline or nortriptyline also treat chronic pain, even in people without depression. These medications affect neurotransmitter levels in ways that can reduce pain signals and improve sleep quality.
Opioid Medications
For severe chronic shoulder pain that doesn’t respond to other treatments, opioid medications may be considered. These powerful pain relievers work on opioid receptors in the brain and spinal cord to reduce pain perception.
Given the current understanding of opioid risks, these medications are typically reserved for specific situations and require careful monitoring. Your doctor will assess your pain severity, functional limitations, and risk factors before considering opioid therapy.
If prescribed, opioids are usually part of a comprehensive pain management plan that includes other treatments. Regular monitoring helps ensure the medications remain effective while minimizing risks of dependence or other complications.
Medication Management Strategies
Successful prescription medication management for chronic shoulder pain often involves trying different approaches to find what works best for you. Your doctor may start with one medication and adjust the dose or switch to different options based on your response.
Combination therapy using medications from different classes can sometimes provide better pain relief than single medications alone. For example, combining an anti-inflammatory with a muscle relaxant might address multiple aspects of your pain.
Regular follow-up appointments allow your healthcare provider to monitor effectiveness and adjust treatments as needed. Keeping a pain diary can help track which medications work best for different activities or times of day.
Side Effect Management
All prescription medications can cause side effects, and your doctor will discuss potential risks before starting any new treatment. Common side effects vary by medication class but may include drowsiness, dizziness, stomach irritation, or dry mouth.
Starting medications at low doses and gradually increasing can help minimize side effects while finding effective pain relief levels. Some side effects improve over time as your body adjusts to the medication.
Your pharmacist can provide valuable information about drug interactions and timing of doses to maximize effectiveness while minimizing side effects. They can also suggest strategies for managing common side effects when they occur.
Working closely with your healthcare team ensures you receive appropriate medication management as part of your comprehensive shoulder pain treatment plan. Regular communication about benefits and side effects helps optimize your treatment while maintaining safety.